Congestive Heart Failure
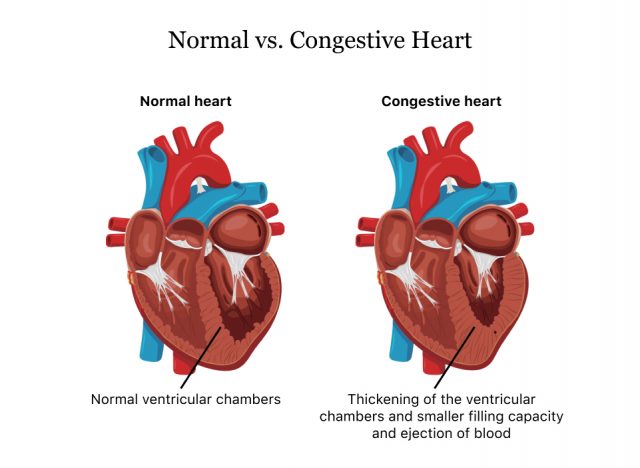
Congestive heart failure, or CHF, is a condition in which the heart no longer pumps enough blood for the body, causing fluid buildup around the heart, lungs and other tissues. People often use the terms “CHF” and “heart failure” interchangeably. But CHF refers to the progressive stages of fluid buildup, and heart failure refers to the heart’s inability to pump enough blood.
About 6.4 million American adults have heart failure, and it was a contributing cause in 1 in 8 deaths in 2017, according to the Centers for Disease Control and Prevention.
Heart failure doesn’t mean your heart has stopped, it just means that it doesn’t pump enough blood. This weakened ability to pump blood causes fluid and blood to back up into the lungs, making it hard to breathe and causing swelling in the ankles, feet and legs.
People who are 65 years or older, people who are overweight, people who have had a heart attack and African Americans are at greatest risk for CHF. It also affects more men than women.
Common Types
Heart failure can affect the left side of the heart, the right side or both. Each type has slightly different symptoms. The type of CHF also affects the type of treatment.
Left-sided Heart Failure
Left-sided heart failure occurs when the left ventricle of the heart no longer pumps enough blood. It’s the most common type of failure. Because of this, the veins that carry blood away from the lungs — the pulmonary veins — build up with blood. When this happens, people may have shortness of breath, trouble breathing or coughing. It gets worse during physical activity.
There are two kinds of left-sided failure.
Systolic Failure or Heart Failure with Reduced Ejection Fraction (HFrEF)
The left ventricle can no longer contract normally, and the heart is too weak to push enough blood into the body.
Diastolic Failure or Heart Failure with Preserved Ejection Fraction (HFpEF)
The left ventricle becomes stiff and loses its ability to relax, and the heart doesn’t properly fill up with blood in between beats.
Right-sided Heart Failure
Right-sided heart failure occurs when the right ventricle cannot pump enough blood to the lungs, causing blood to build up in the veins that bring blood to the lungs. This causes fluid to leak out from the veins into the surrounding tissues. Fluid usually builds up in the legs, but sometimes it can also build up in the belly or genital area.
Biventricular Heart Failure
Failure in both sides of the heart is called biventricular heart failure. This type combines the symptoms of both left and right heart failure.
Four Stages of CHF
Congestive heart failure has four stages. It begins with stage I — sometimes called class I or pre-heart failure. It then progresses over time to stage IV, sometimes called class IV or advanced heart failure.
Treatment recommendations and symptoms are different depending on the stage.
| Stage | Symptoms | Treatment and Management |
|---|---|---|
| I | There are often no symptoms, and daily life isn’t affected. But sometimes people will begin having trouble breathing when lying down because of fluid buildup. | At this stage, CHF can be managed with lifestyle changes and some medication. |
| II | Shortness of breath, palpitations and fatigue during activity and routine chores. | Management is similar to stage I but with more monitoring. |
| III | Physical activity leads to more severe stage II symptoms. Simple tasks like walking to the mailbox cause extreme respiratory distress. | People will have to work closely with their health care provider to manage symptoms and discuss treatment plans. |
| IV | Advanced heart failure. Physical activity is almost impossible and people may be confined to sitting on chairs and sleeping in upright beds. | At this stage, treatment is focused on increasing a person’s comfort. |
Congestive Heart Failure Symptoms
Signs of heart failure can appear in anyone at any age, even in young children that may be born with heart defects. But it usually affects older people with weakened hearts from other diseases.
There may be no symptoms in the early stages, but people start having symptoms in stage II and they get progressively worse, especially without treatment.
- Bluish skin and rapid breathing
- Breathing spasms and wheezing similar to asthma
- Disorientation, brain fog, confusion that’s more pronounced in older people
- Fainting, dizziness, weakness or fatigue
- Getting tired easily
- Feelings of anxiety, suffocation and restlessness
- Hacking, dry cough that happens more often when lying down
- Having to urinate more often at night
- Lung congestion and difficulty breathing from blood backing up into the lungs
- Nausea, abdominal swelling, tenderness or pain (may result from the buildup of fluid in the body and the backup of blood in the liver)
- Swelling (edema) from fluid buildup, especially in the feet, ankles and legs
- Weight gain from fluid buildup or weight loss from poor nutrient absorption and decreased appetite
Causes and Risks
Congestive heart failure is usually caused by another disease or health condition. This is especially true of conditions that cause damage to the heart or make it work harder than it should. The most common health problems that may cause heart failure are high blood pressure, coronary artery disease and previous heart attack.
- Anemia
- Constrictive pericarditis
- Heart muscle parasites
- Heart valve disorders
- Kidney failure, which causes fluid to build up in the blood stream, making it harder for the heart to work
- Myocarditis
- Narrowing or hardening of the arteries, coronary artery disease
- Previous heart attack
- Problems in the heart's electrical conduction system
- Pulmonary embolism or blood clot in the lungs
- Some lung disorder types
- Thyroid problems that speed up or slow down the pumping of the heart
- Type 2 diabetes
- Untreated high blood pressure
Risk Factors
One in five Americans will develop heart failure, according to the American Heart Association. Certain people are more at risk of developing the disease. Some of these risks, such as keeping a healthy weight, are changeable. Other risks, such as genetics, are not.
Age
The heart muscle weakens with age and people over 65 are most likely to have heart failure. They may also have more health conditions that make them susceptible to heart failure.
Race
Among all races, African Americans have the highest rate of heart failure. They tend to have symptoms younger, have more deaths from heart failure and also have more hospital visits because of the disease.
Weight
Overweight or obese people have a greater risk of heart failure because excess weight puts strain on the heart. People who are overweight also have a greater risk of Type 2 diabetes and heart disease — both conditions can lead to heart failure.
Previous Heart Attack
People who have had a previous heart attack have weaker heart muscles. This can lead to heart failure.
Genetics
Heart failure can run in families. Children born with heart defects are also at risk for heart failure.
Medications That Cause or Worsen CHF
In addition to health problems, some medications may cause or worsen CHF. Be sure to tell the doctor about all medications you take.
- Painkillers (NSAIDs and COX-2 inhibitors)
- Anesthesia medications (desflurane, enflurane, halothane and others)
- Diabetes medications (metformin, Onglyza (saxagliptin), Januvia (sitagliptin), Actos (pioglitazone), Avandia (rosiglitazone))
- Doxazosin
- Verapimil
- Monoxidil
- Antifungal medications (itraconozole)
- Some chemotherapy agents including Taxotere (docetaxel)
- Antidepressants such as Celexa (citalopram)
- Antiparkinson medications
- Antimigraine medications
- Bipolar medications such as lithium
Diagnosing CHF
A cardiologist is typically the specialist who can diagnose CHF. The doctor will ask the patient about any symptoms they may be having, such as swelling or shortness of breath. It’s important to tell the doctor if you have other health conditions such as heart disease, high cholesterol, high blood pressure, kidney disease and diabetes.
Along with a physical exam, the doctor may order tests to check for CHF.
CHF Tests
These tests help the doctor figure out what caused the heart failure. They can also rule out heart failure. Many of them are geared toward looking at how the heart is functioning and its pumping strength.
Blood Tests
Doctors will order blood tests for anemia and kidney or thyroid problems. The symptoms of these conditions may mimic heart failure. The doctor will also check cholesterol levels.
NT-pro B-type Natriuretic Peptide (BNP)
People with heart failure have high levels of BNP in the blood — a hormone released by the lower chambers of the heart (ventricles). Depending on the severity of heart failure, the levels of levels of NT-pro BNP change. Higher levels mean the ventricles are more stressed. People with a level of more than 450 picogram/milliliter(pg/mL) — one trillionth of a gram per milliliter — for patients under age 50 or 900 pg/mL for patients 50 and older may signify heart failure.
Cardiac Catheterization
Doctors insert a long, thin tube called a catheter into an artery in the leg or arm. Sometimes doctors also insert dye to record videos of the heart valves, chambers and blood vessels. This can show how well the heart is pumping.
Chest X-ray
An X-ray can show fluid buildup around the lungs and heart and how big the heart muscle is.
Echocardiogram (echo)
An echo is an ultrasound that can show how well the heart pumps, the function of the valves, the blood flow and the heart’s size. It can measure the pressure in the heart and the ejection fraction (EF) — a measurement of the blood pumped out of the heart with each beat.
Ejection fraction (EF)
EF measures how much blood the heart pumps with each beat. Doctors can test for EF using several methods: echocardiogram (echo), magnetic resonance imaging (MRI), multigated acquisition (MUGA) scan, during a heart catheterization and during a nuclear stress test. Normal EF is between 55% and 70%. This can change depending on how well heart failure is managed and treated. This can also help diagnose the stage of heart failure and tell the doctor how well treatment is working.
Electrocardiogram (EKG or ECG)
Doctors use this test to check the heart’s electrical activity. Electrodes are connected to wires connected to sticky patches placed on a person’s body. Information from electrodes creates a graph on a monitor. Abnormal heart rhythms may signal heart failure.
Multigated Acquisition Scan (MUGA scan)
In this test, a special camera called a gamma camera creates a video of the heartbeat and how the ventricles work after the health care provider injects a small amount of radioactive dye into a vein.
Stress Test
A stress test shows doctors how the heart reacts to activity and stress. Patients may get on a treadmill or bike while blood pressure, heart rate and electrocardiograph are measured. People who cannot exercise may take a drug that mimics exercise.
Treatment
Treatment plans for CHF focus on stopping or slowing disease progression because there is no cure for CHF. Once a person progresses to the next stage, there is no reversing it. Cardiologists are specialists that develop treatment plans for people with CHF.
Medication is the main treatment for CHF and people with the condition typically have to take medicines for the rest of their lives to stay healthy. Patients should speak to their health care provider right away if they develop side effects.
If medication fails to help, patients may benefit from surgery to repair heart valves or clear blood vessels.
ACE Inhibitors
Angiotensin converting enzyme (ACE) inhibitors dilate blood vessels to lower blood pressure and lessen the workload on the heart. They also lower the amount of heart-damaging hormones.
Drugs in this class include Prinivil (Lisinopril) and Capoten (captopril). Common side effects include dizziness, increased potassium levels, drug cough and changes in kidney function. Patients should get regular blood tests to check kidney function.
Angiotensin II Receptor Blockers (or Inhibitors)
These drugs work similarly to ACE inhibitors, but dry cough side effects are less severe.
Drugs in this class include Diovan (valsartan) and Cozaar (losartan). Like ACE inhibitors, these drugs may damage kidneys so tests for kidney functions are recommended. Common side effects include dizziness, changes in kidney function and increased potassium levels.
Beta Blockers
These drugs cause the heart to beat more slowly and with less force. They also lower blood pressure.
Drugs in this class include Toprol (metoprolol) and Coreg (carvedilol). Common side effects are fatigue, dizziness, drowsiness, headache and upset stomach. Don’t stop taking a beta blocker without talking to a health care provider.
Diuretics
People sometimes call diuretics “water pills” because they work by removing excess fluid from the body. Because diuretics cause the body to lose potassium, people may need to take potassium supplements.
Drugs in this class include Lasix (furosemide), Bumex (bumetanide) and Zaroxolyn (metolazone). Common side effects include dizziness, increased urination, skin rash, changes in kidney function, increased blood sugar levels, gout and dehydration.
Aldosterone Antagonists
These medications work by stopping the body from making too much aldosterone, a hormone that can damage the heart.
Drugs in this class include Inspra (eplerenone) and Aldactone (spironolactone). Common side effects include breast swelling or tenderness in men and women, increased potassium and changes in kidney function. Patients should get routine kidney and potassium tests.
Digoxin
This drug slows the heart rate and may improve the heart’s pumping ability. Blood tests are needed to find the right dose. Common side effects include digestive problems, poor appetite and nausea.
Isosorbide Dinitrate/Hydralazine Hydrochloride
This medicine helps relax blood vessels and reduce the strain on the heart. These drugs are primarily helpful for treating heart failure in African Americans, and studies have shown the medicine can reduce the risk of death, according to the National Heart, Lung and Blood Institute.
Common side effects include dizziness, headache and swelling in the extremities.
Preventing and Living with CHF
Because heart failure is a serious, progressive condition, prevention is important. For people living with CHF, there are things they can do to stop or slow disease progression and improve their quality of life.
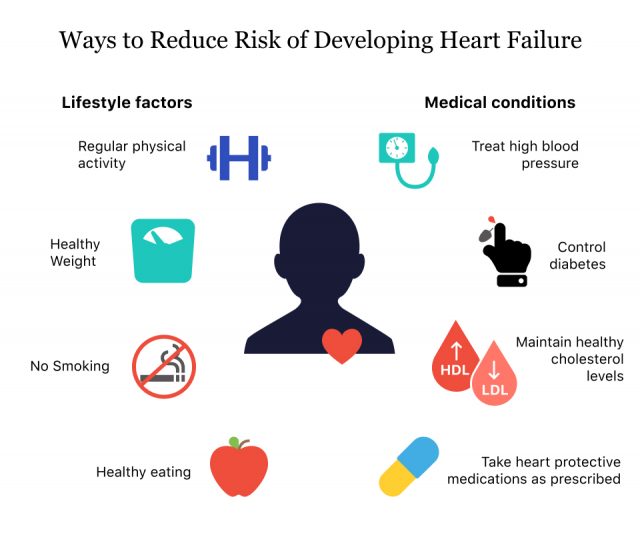
Prevention
The main way people can prevent CHF is by maintaining good cardiovascular health.
“To avoid heart failure, there’s a need to prevent other heart problems.”
“To avoid heart failure, there’s a need to prevent other heart problems,” Johns Hopkins cardiologist Dr. Steven Jones said.
- Exercise at least 5 days a week
- Maintain a healthy body weight
- Don’t smoke
- Eat more fruits and vegetables
- Eat fish
- Limit alcohol intake to 1 drink a day or avoid it
- Don’t drink more than 4 cups of coffee a day
- Don’t use illegal drugs
- Talk to your doctor about medications that may increase CHF risk
- Treat any existing conditions that may lead to CHF
Congestive Heart Failure Prognosis
CHF prognosis depends on the stage of disease, what caused the disease and how effective the treatment is.
In general, people with class I or II CHF have the best prognosis. People with heart failure caused by coronary artery disease or primary cardiomyopathy had worse survival rates than people with other causes, according to researcher M. Matoba and colleagues at the Kanazawa Medical University in Japan.
- 1 Year, 78.5 percent
- 3 Year, 59.8 percent
- 5 Year, 50.4 percent
- 10 Year, 14.7 percent
Source: Japanese Circulation Journal
Improving Quality of Life
Currently, CHF has no cure. People living with the disease have to commit to heart-healthy lifestyles and take medication regularly.
To stay healthy, here are some tips to follow.
- Monitor symptoms and check for sudden weight gain and swelling in legs and feet.
- Monitor blood pressure and weight and get lab work done regularly to be aware of your heart health and disease progression.
- Stay positive and find ways to alleviate stress including finding relaxing hobbies, talking to a therapist, finding a support group or talking to loved ones and friends.
- Ask questions about the stage of your disease and guidelines for how active you should be. This includes work, sex and exercise. Depending on the stage of disease, your doctor will have different recommendations about how active you should be, including work, sexm and exercise.
- Keep all appointments with your doctors.
- Make all the lifestyle changes your doctor recommends. If you need help with your diet, ask to see a nutritionist or dietician.
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.

