Bipolar Disorder
Bipolar disorder, formerly known as manic depression, is a mental disorder that causes extreme highs and lows in mood known as mania and depression. These highs and lows affect a person’s energy and concentration and make it difficult to perform daily tasks. Treatment options include psychotherapy, medication and lifestyle changes.
People with bipolar disorder can feel like they are on an emotional roller coaster, but they aren’t alone. About 2.8 percent of American adults experience bipolar disorder each year, according to the National Institutes for Mental Health. As many as 10 million adults and children have this type of mental health disorder in the United States, according to an article in JAMA.
Bipolar disorder usually affects younger people, and it starts in the late teens or early adulthood. The median age of onset is 25, but people older or younger can manifest symptoms.
Episodes of mania or depression may occur rarely or multiple times a year with emotional symptoms in between episodes.
People with bipolar disorder have an increased risk of thyroid disease, heart disease, diabetes, headaches and migraines. The majority of people, about 83 percent, suffer serious impairment because of the disorder, which can get worse if left untreated.
Bipolar disorder has no cure, but with the right treatment people can manage their mood swings and improve their quality of life.
Types of Bipolar Disorder
There are three types of bipolar disorder. Each type varies in the severity and duration of symptoms.
Bipolar I
People diagnosed with bipolar I disorder experience manic episodes that last at least seven days. Some episodes may not last seven days, but they can be severe enough to require hospitalization. In addition, people may suffer symptoms of depression that can last two weeks. But depression isn’t necessary for a diagnosis.
During a manic episode, people with bipolar I have increased energy, may talk too fast or jump from one topic to the other, according to Dr. Anthony Rothschild, a professor of psychiatry at the University of Massachusetts Medical School.
Rothschild told U.S. News and World Report that people with bipolar I also have feelings of strong euphoria or irritability. Mania may also manifest in delusions that require hospitalization.
Bipolar II
The main difference between bipolar I and II is the severity of the manic episodes. People with bipolar II disorder have more serious symptoms of depression and cycle between these symptoms and hypomania — a less severe type of mania.
Hypomania lasts about four days — as opposed to full-blown mania that lasts at least seven. Hypomanic episodes rarely lead to hospitalization and people with this condition can still function.
People with hypomania generally feel energetic, have a good mood, sleep less and have periods of increased productivity. But they can face personal issues at home or work and make impulsive decisions because of hypomania.
Cyclothymic Disorder (Cyclothymia)
People with cyclothymia experience periods of hypomanic symptoms and depressive symptoms that last at least two years. These symptoms are much less severe but are more chronic in nature.
The highs experienced with cyclothymia include agitation, being easily distracted, having racing thoughts or engaging in risky activities such as spending sprees or sexual encounters. Lows may include feelings of social isolation, guilt, insomnia or difficulty concentrating.
Advertisement
Professional Therapy, Done Online
A licensed therapist with BetterHelp can provide professional support and guidance, on your schedule. Sign up and get matched in as little as 48 hours.
Get Started
Symptoms of Mania and Depression
People with bipolar disorder can feel like they are on top of the world one minute and at their worst the next. These extreme highs and lows of mania and depression are called mood episodes. But sometimes they experience symptoms of both in one episode.
The length of an episode varies by person, but the median duration of bipolar I mood episodes is about 13 weeks, according to a study by David A. Solomon and colleagues published in JAMA Psychiatry.
Researchers found that more than 75 percent of the study participants experienced recovery within one year of the onset of a mood episode. People recovered more quickly from mania or hypomania than they did from major depressive episodes.
| Manic Episodes | Depressive Episodes |
|---|---|
| Show poor judgment and have risky behaviors such as over eating or drinking, have reckless sex or spend excessively | Lack of interest in hobbies or activities, inability to experience pleasure, decreased sex drive |
| Feelings of jumpiness or extreme energy | Feelings of restlessness or being slow |
| Racing thoughts | Difficulty concentrating |
| Have overblown feelings of self-esteem, feeling important or powerful | Feeling worthless, guilty or have thoughts about death or suicide |
| Extreme elation or irritability | Hopelessness or worry |
| Sleep very little, insomnia | Too much sleep, or have difficulty falling asleep |
| Decreased appetite | Eat more and experience weight gain |
| Speak quickly, jump from one topic to another | Feelings of nothing to say or slow speech, forgetfulness |
| Multitasking and increased productivity | Lack of motivation, unable to do simple things |
National Suicide Hotline
1-800-273-8255
https://suicidepreventionlifeline.org
Crisis Textline
Text “HELLO” to 741741
www.crisistextline.org
911
Go to the nearest hospital emergency room or call 911
Risks and Causes
Researchers haven’t pinpointed one cause of bipolar disorder. Several environmental and physical factors may lead to developing the disorder.
- Family History and Genetics
- Research shows that bipolar disorder runs in families. For example, if a person’s parent has the disorder, they have a 10 to 15 percent greater chance of developing it. People with certain genes are also more likely to have the disorder.
- Brain Structure
- Researchers have found that there are subtle differences in brain size and how the brains of people with bipolar disorder work. For example, brain MRI studies showed that people with bipolar respond to visual stimuli differently, according to Brain & Behavior Research Foundation.
- Stress
- Stressful events may trigger depressive or manic mood episodes. Examples include a death in the family, financial problems, difficult relationships or divorce.
- Drug Use
- Prescription and illicit drugs may trigger manic episodes in people susceptible to bipolar disorder. These include antidepressants, corticosteroids, amphetamines like ecstasy and cocaine, and excessive caffeine.
Advertisement
Real Therapy, Done Online
BetterHelp offers flexible scheduling so you can make time for therapy in between meetings, classes, child care, and more. Get 20% off your first month.
Get Started
Getting a Diagnosis
Health care providers conduct interviews, physical examinations and lab tests to diagnose bipolar disorder. The blood tests can rule out other medical problems that have similar symptoms such as thyroid disease or multiple sclerosis.
Diagnosing bipolar disorder can be difficult. Studies show about 40 percent of people with bipolar disorder are initially misdiagnosed with major depressive disorder because onset of the condition usually begins with depressive symptoms, according to an article by Drs. Tanvir Singh and Muhammad Rajput.
Proper diagnosis requires long-term observation and careful documentation of symptoms. Health care providers may collect information from friends, family and significant others to get a more accurate picture of symptoms and how long they last.
Bipolar Disorder vs. Depression
The main distinction between bipolar disorder and depression — also called clinical depression or major depressive disorder — is that people with bipolar also experience the extreme highs of mania or hypomania in addition to the lows of depression.
Bipolar disorder is also rarer than depression, which affects over 17 million American adults, according to the Depression and Bipolar Support Alliance.
Some studies also show that symptoms of depression in people with bipolar disorder I or II are more severe.
Bipolar Disorder Tests
Health care providers may also use tests such as the Mood Disorder Questionnaire, or MDQ, to help screen people for bipolar disorder. The MDQ consists of 13 yes or no items for patients to answer. The questionnaire has shown good sensitivity and specificity in diagnosing bipolar I, though it is not as effective with bipolar II, according to Singh and Rajput.
In general, people who screen positive for bipolar answer “Yes” to 7 or more of the 13 items in Question 1, answer “Yes” to Question 2 and answer “Moderate Problem” or “Serious Problem” to Question 3.
This questionnaire is for screening purposes only and should not be used as a diagnostic tool.
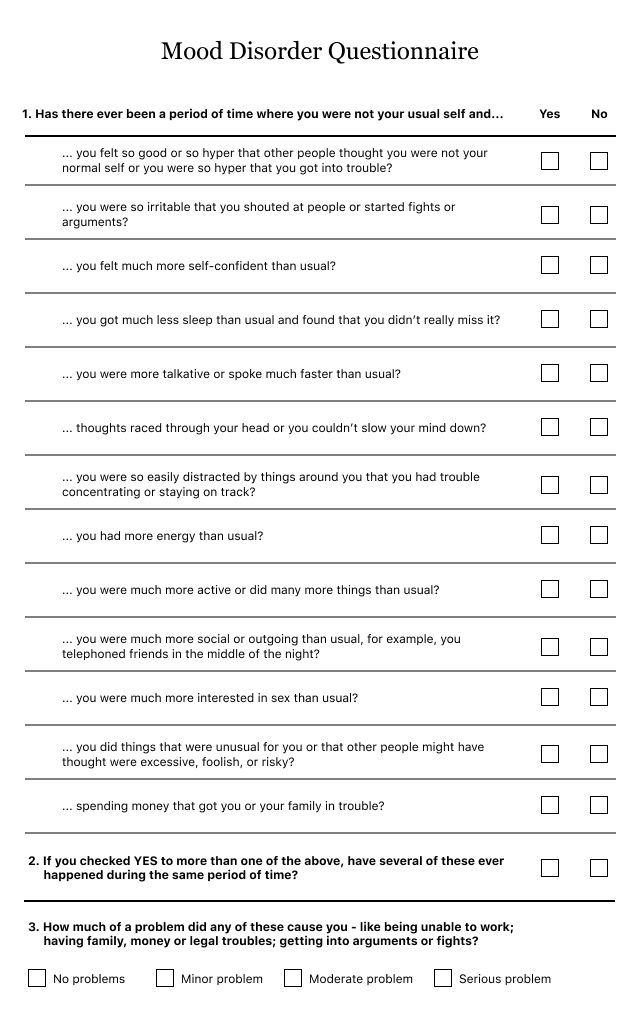
Source: International Bipolar Foundation
Medication, Psychotherapy and Other Treatments
The most effective treatment for bipolar disorder combines medication and psychotherapy. Therapies that stimulate the brain and combine lifestyle changes may also be beneficial.
For some patients, it can be difficult to find effective treatment and it’s often a trial and error process. For example, John R. Geddes and David J. Miklowitz found that about 37 percent of patients relapse into depression or mania within 1 year, even with treatment. Depressive symptoms are more likely to reoccur than manic symptoms.
Patients should continue to work with their health care providers to find the most effective combination of treatments and adhere to the plan to avoid any relapses.
Medication
There are several medications approved by the U.S. Food and Drug Administration to treat bipolar disorder. These include mood stabilizers and antipsychotic drugs, including atypical antipsychotics.
Although people with bipolar disorder have symptoms of depression, they can’t use the same medications as people with major depression because antidepressants such as selective serotonin reuptake inhibitors, or SSRIs, may trigger manic symptoms, according to the FDA.
Common side effects of medications for bipolar disorder include nausea, dizziness, sleepiness, fatigue, feeling restless, increased thirst and trembling.
Pregnant women should discuss the risks and benefits of taking medication while pregnant because there aren’t enough studies to determine safety or effectiveness.
Medications for Bipolar Disorder
- Abilify (aripiprazole)
- Saphris (asenapine maleate)
- Clozaril (clozapine)
- Fanapt (Iloperidone)
- Latuda (lurasidone)
- Zyprexa (olanzapine)
- Symbyax (olanzapine/fluoxetine)
- Invega (paliperidone)
- Seroquel (quetiapine)
- Risperdal (risperidone)
- Geodon (ziprasidone)
- Lithium
- Depakote (valproate)
- Tegretol (carbamazepine)
Psychotherapy
While medication may be the first line of treatment for bipolar disorder, some studies show that medication alone results in high rates of recurrence, according to researchers Holly A. Swartz and Joshua Swanson.
Swartz and Swanson found that people who used bipolar-specific psychotherapy with medication had better results than those who did not. The researchers published their findings of several types of psychotherapy for bipolar disorder in the psychiatric journal Focus.
- Cognitive Behavioral Therapy (CBT)
- This treatment helps people recognize and modify the way they think and act to reduce episodes of mania and depression. Studies have shown CBT increases the length of time between mood episodes, according to Swartz and Swanson. A 2018 review published by the U.S. Department of Health & Human Services Agency for Healthcare Research and Quality found that CBT may not have an advantage over other psychotherapies.
- Family-focused Therapy (FFT)
- Family-focused therapy focuses on training patients on how to better communicate and problem solve. This therapy also involves a family member, usually a parent or sibling. Swartz and Swanson found that FFT hastened recovery and help protect a person against recurrence.
- Interpersonal and Social Rhythm Therapy (IPSRT)
- Interpersonal and Social Rhythm Therapy (IPSRT) helps patients better interact with others and schedule their daily activities, such as eating, sleeping and work or school. The theory is that having a routine will help regulate biologic rhythms and reduce mood episodes. Swartz and Swanson found that this type of therapy is effective to control acute episodes and as maintenance treatment.
Brain Stimulation Therapies
Electroconvulsive Therapy (ECT) — once called electroshock therapy — and Deep Brain Stimulation (DBS) use electric currents to stimulate the brain and treat symptoms of bipolar disorder. While these treatments have shown some promise, most are still experimental for treating bipolar disorder.
ECT can be effective at treating manic and depressive episodes in people who do not respond to medication and psychotherapy, according to the National Institute for Mental Health. It is administered under anesthesia and may be helpful to prevent suicide or when a patient is unresponsive.
Side effects of ECT include headaches, muscle pain, memory loss, and confusion. Side effects of DBS include speech problems, mood swings, brain bleeding, insomnia and breathing problems.
Sleep and Exercise
Getting enough sleep and exercise in addition to medication and psychotherapy can help manage mood swings and prevent triggering episodes.
Missing sleep or getting too much sleep can trigger an episode. Try to go to bed and wake up at a regular time. Avoid eating, exercising and using electronic devices too close to bedtime.
Exercise is proven to help improve moods. A review in Journal of Affective Disorders found that exercise generally improved health and lessened depressive symptoms in patients with bipolar disorder, but also found a relationship between vigorous exercise and mania.
Differences Between Men and Women
Men and women experience bipolar disorder differently, though both genders have similar rates of the disorder.
Women are more likely to have bipolar II, and the onset is later than in men.
Females with bipolar disorder may also have other co-occurring medical problems such as thyroid disease, obesity, migraine and anxiety disorders.
In contrast, substance abuse disorder more often co-occurs in men, and they are less likely to adhere to treatments. Men may also have problems with the law or alcohol abuse.
Menstrual cycles may also affect symptoms in women. For example, some women have worse symptoms during their period.
Childbirth may trigger symptoms. It’s a high-risk time for onset or recurrence of bipolar disorder, and the risk for mood episodes increases during the postpartum period.
Women with bipolar disorder are two to three times more likely to attempt suicide, but men are two to three times more likely to succeed, psychologist Cynthia G. Last told PsychCentral.
Children and Teens
About 3.4 million children and teens suffer from depression in the U.S., and about one third of them may have bipolar disorder, according to Mental Health America.
Teens ages 17-18 have a higher rate of the disorder than younger children do, and the prevalence is higher in females.
Children and teens experience the same ups and downs as adults with bipolar disorder. They may have problems at school or trouble interacting with friends and family members. Young people may also attempt suicide.
In young people, the disorder may co-occur with other mental health issues such as substance abuse, ADHD or anxiety disorders.
Sometimes a child’s disorder changes and treatment has to be adjusted. For example, a health care provider may need to change medications or the dose of a current medication.
- Keep track of the child’s moods, sleep patterns and behaviors to better understand the illness and track effectiveness of treatment.
- Help the child understand how treatment can help them.
- Encourage the child to share how they feel.
- Have patience.
- Encourage the child to have fun.
- Find a support group for caregivers of children with bipolar disorder.
- Practice self-care to keep stress levels down.
- Find someone to talk to like a friend or therapist.
Living with Bipolar Disorder
Coping with bipolar disorder can be difficult, but you can do a few things to make it easier for yourself and loved ones.
- Avoid abusing drugs and alcohol.
- Follow your treatment plan, including sticking to medications and psychotherapy.
- Communicate your feelings and reach out for help.
- Keep a routine with sleep, meals and work or school.
- Keep a journal of your moods and pay attention to things that trigger episodes.
- Be patient with yourself and the process of getting better, it may take a while to find what works but don’t give up.
- Keep all therapy appointments.
- Get help right away if you are thinking of harming yourself.
- Have a support system in place for mood episodes.
- If something isn’t working for you, talk to your health care provider.
Advertisement
Professional Therapy, Done Online
A licensed therapist with BetterHelp can provide professional support and guidance, on your schedule. Sign up and get matched in as little as 48 hours.
Get Started
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.




