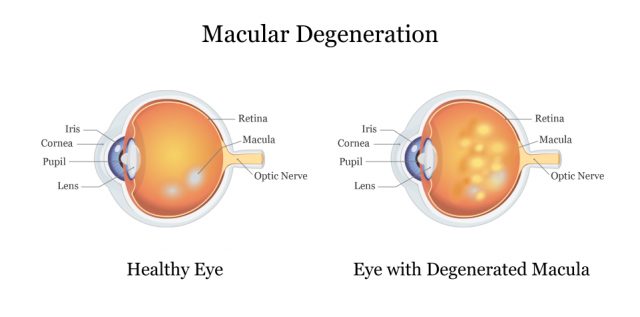
Macular Degeneration
Macular degeneration, also called age-related macular degeneration or AMD, is an eye disease that gradually destroys central vision. It causes blurry vision, and is the leading cause of vision loss in Americans ages 60 and older.
Macular degeneration occurs when deposits called drusen build up in the eye. These deposits cause light-sensitive cells to die off or blood vessels to leak and cause cell damage.
It’s more common in white Americans. Eighty-nine percent of people who get macular degeneration are white, and about 14% of white Americans ages 80 or older have the disease, according to the National Eye Institute.
There are two types of macular degeneration: dry and wet. Dry AMD is the most common and makes up 85 to 90% of cases, according to the American Macular Degeneration Foundation.
Researchers don’t know exactly what causes macular degeneration, but the biggest risk for developing it is increased age. There is no cure for macular degeneration, and treatments focus on preventing or slowing down eye damage.
Macular Degeneration and Elmiron
New studies show that people who take Elmiron for an extended period of time have an increased risk of developing pigmentary maculopathy. This includes loss of central vision, blurry or distorted vision, loss of color vision, or impaired depth perception.
In July 2019, Drs. Adam M. Hanif and Nieraj Jain published their study on Elmiron and pigmentary maculopathy in Review of Ophthalmology. Study authors called the eye damage “preventable, vision-threatening medication toxicity that could masquerade as other known maculopathies.”
“Our subsequent investigations demonstrated that this unique maculopathy is strongly associated with chronic PPS exposure, not [interstitial cystitis] IC itself or its other therapies. In fact, this characteristic maculopathy has, to date, been exclusively diagnosed in patients reporting prior PPS exposure,” the authors wrote.
After reading the findings of Hanif and Jain, Drs. Robin A. Vora, Amar P. Patel and Ronald Melles at Kaiser Permanente looked at Kaiser Permanente’s database of 4.3 million patients and presented their findings in October 2019.
They found 140 patients who took an average of 5,000 Elmiron pills over 15 years. Ninety-one of those patients came in for an exam, and 22 of those patients showed clear signs of eye damage and drug toxicity.
A 2022 review of the literature confirms the consensus around this disease: higher cumulative doses of pentosan cause maculopathy with symptoms consistent with rod dysfunction, similar to age-related macular degeneration.
Symptoms of Elmiron Eye Damage
Common symptoms of Elmiron eye damage in the Hanif and Jain study were blurred vision while reading, taking a long time to adjust to dark lighting, and metamorphopsia, a visual defect that causes lines to look curvy or round.
How Long Did It Take to Develop Vision Problems?
The median duration of Elmiron use was about 14.5 years among patients in the Hanif and Jain study. But symptoms could occur as early as three years after starting Elmiron treatment.
Patients showed signs of vision damage that lasted from one to nine years at the time of the study. Vision damage may be permanent. Patients who took Elmiron and experienced vision damage as a result are currently filing Elmiron lawsuits.
Alternatives to Elmiron
Elmiron is the only oral medication approved to treat symptoms of IC — a condition that causes bladder pressure and pain. But there are alternatives to Elmiron that may help manage the symptoms of IC in people who stop taking drug.
- Lifestyle Changes
- Stay away from food or drink that triggers symptoms. Ask your doctor about a diet that may help control symptoms. Be sure to drink enough water to prevent dehydration. Stop smoking, reduce stress and stay physically active.
- Bladder Training
- Bladder training to hold more urine may help with urinary urgency and pain.
- Bowel Training
- Some people find that training their bowel to have more regular movements helps their IC symptoms.
- Physical Therapy
- People with IC symptoms that include pelvic muscle spasms may see a physical therapist to stretch tight muscles and help them relax.
- Pain Relievers
- Pain relievers such as ibuprofen, aspirin or Tylenol (acetaminophen) may control IC pain. For stronger pain, doctors may prescribe stronger medications.
Living with Macular Degeneration
There is no cure for macular degeneration but some treatments may slow disease progression. People can make lifestyle changes to help them cope with vision loss and help prevent disease progression.
- Don’t smoke
- Eat a healthy diet
- Have your eyes checked regularly
- Keep your cholesterol and blood pressure down
- Protect your eyes from the sun when outdoors by wearing sunglasses or hats
- Get rid of furniture and clutter that may cause you to trip
- Use good lighting when reading
- Ask your doctor about optical devices such as magnifying glasses to help you see better
- Seek the support of family and friends or a support group
- Use alternative forms of travel to get around such as Uber, taxis, buses and trains
Supplements
Some supplements may help people with age-related macular degeneration, according to the American Macular Degeneration Foundation. Supplements are especially helpful for people who have signs of macular degeneration, a family history of the disease or those who don’t eat enough greens or fish.
Always check with your doctor before taking any supplements because they may interact with other medications.
- Lutein, 6-10 mg
- Omega-3 fatty acids, 1000 mg (fish oil) if not eating fish
- Vitamin C, 500 mg
- Vitamin D3, 1000 – 2000 IU
- Vitamin E, 200 – 400 IU
- Zeaxanthin, 2 mg
- Zinc, 20 – 80 mg
What Is the Best Treatment for Macular Degeneration?
There is no cure for macular degeneration, and each person may respond to treatment differently. Each treatment plan is tailored to the individual depending on the type and stage of AMD.
Early stage AMD has no treatment beyond lifestyle changes such as healthy diet and exercise. But research from the National Eye Institute shows that special supplement formulas called AREDS and AREDS2 may slow vision loss when taken daily.
These formulas contain beta-carotene, vitamin C, vitamin E, copper, lutein, Zeaxanthin and zinc. The AREDS formula is not recommended for current or former smokers.
People with late stage or wet AMD have two options to slow down or stop vision loss: photodynamic therapy, or PDT, and anti-VEGF injections.
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.