Food and Drug Administration (FDA)
The U.S. Food and Drug Administration’s original purpose was to regulate the selling of misbranded food and drugs. Over the years, the agency’s role grew to include the approval and regulation of medical devices in addition to pharmaceuticals. It also supervises drug, device and vaccine recalls. The agency collects reports of adverse events and warns the public when needed.
Our content is developed and backed by respected legal, medical and scientific experts. More than 30 contributors, including product liability attorneys and board-certified physicians, have reviewed our website to ensure it’s medically sound and legally accurate.
legal help when you need it most.
Drugwatch has provided people injured by harmful drugs and devices with reliable answers and experienced legal help since 2009. Brought to you by The Wilson Firm LLP, we've pursued justice for more than 20,000 families and secured $324 million in settlements and verdicts against negligent manufacturers.
More than 30 contributors, including mass tort attorneys and board-certified doctors, have reviewed our website and added their unique perspectives to ensure you get the most updated and highest quality information.
Drugwatch.com is AACI-certified as a trusted medical content website and is produced by lawyers, a patient advocate and award-winning journalists whose affiliations include the American Bar Association and the American Medical Writers Association.
About Drugwatch.com
- 15+ Years of Advocacy
- $324 Million Recovered for Clients
- 20,000 Families Helped
- A+ BBB Rating
- 4.9 Stars from Google Reviews
Testimonials
I found Drugwatch to be very helpful with finding the right lawyers. We had the opportunity to share our story as well, so that more people can be aware of NEC. We are forever grateful for them.
- Medically reviewed by Mireille Hobeika, Pharm.D.
- Last update: September 5, 2023
- Est. Read Time: 13 min read
- FDA Organization and Regulation
- How the FDA Regulates and Approves Drugs
- Medical Device Regulation and Approval
- How FDA Conducts Recalls
- How FDA is Funded
- Adverse Event Reporting
- FDA and Clinical Trials
- FDA Scandals and Controversy
- FDA Hides Evidence of Fraud in Clinical Trials
- FDA Milestones & History
The U.S. Food and Drug Administration (FDA) is the government agency responsible for reviewing, approving and regulating medical products, including pharmaceutical drugs and medical devices. It also regulates various other products, including food, cosmetics, veterinary drugs, radiation-emitting products, biological products and tobacco.
The agency’s origins began with the passage of the 1906 Pure Food and Drugs Act, a law created to curb manufacturer abuses in the consumer product marketplace. It was officially named the Food and Drug Administration in 1930.
The FDA’s regulation responsibilities include working with manufacturers to recall problematic products and collecting reports on adverse events—injuries or side effects caused by drugs, devices and vaccines. Manufacturers, doctors and patients may report adverse events to the FDA. If the agency decides these reports are serious, it may issue a safety communication to the public.
“Americans receive as many as 3 billion prescriptions for pharmaceuticals each year, and millions receive medical devices such as hip and knee implants. All medications and medical devices come with inherent risks, but it is the FDA’s duty to address serious risks that can be avoided and managed.”
But even with a system in place to ensure a new or existing product’s safety and minimize its risks, unexpected complications can arise.
Critics and consumer watchdog groups accuse the FDA of being too influenced by Big Pharma and denounced major deficiencies in the FDA system for ensuring the safety of drugs in the U.S. market. They also say the current FDA method for clearing medical devices for sale, the 510(k) premarket approval process, allows untested devices to harm consumers.
As a result, the public’s approval of the FDA has steadily declined. In 2015, only about half of Americans thought the FDA was doing a good job of protecting the public. In 2022, one study in JAMA Network Open found that most Americans want the FDA to be more transparent about drug approvals, clinical trials, drugs that have been discontinued and more.
FDA Organization and Regulation
The FDA is an agency within the U.S. Department of Health and Human Services. Because it regulates a wide variety of products, it is broken down into five different offices: Office of the Commissioner, Office of Foods and Veterinary Medicine, Office of Global Regulatory Operations and Policy, Office of Medical Products and Tobacco and Office of Operations.
In addition to the 50 states, the FDA’s responsibilities extend to the District of Columbia, Puerto Rico, Guam, the Virgin Islands, American Samoa, and other U.S. territories and possessions.

- Protecting the public health by ensuring the safety, effectiveness and security of human and veterinary drugs, medical devices, vaccines and biological products
- Providing the public with accurate, science-based information to ensure the safe and appropriate use of medical products and foods
- Ensuring the safety and proper labeling of food
- Regulating the manufacturing, marketing, and distribution of tobacco products to protect the public health and to reduce tobacco use by minors
- Protecting the public from radiation released by certain electronic products
Office of Medical Products and Tobacco
While the FDA oversees a number of products, it gets the most scrutiny for its regulation of prescription drugs and medical devices. This responsibility falls to the Office of Medical Products and Tobacco. The Office of Medical Products and Tobacco is made up of six centers.
Center for Biologics Evaluation and Research (CBER)
Center for Biologics Evaluation and Research (CBER) regulates biologics such as blood products, tissue products and vaccines.
Center for Devices and Radiological Health (CDRH)
Center for Devices and Radiological Health (CDRH) regulates medical devices such as knee and hip implants and radiation-emitting products such as MRIs and X-ray machines.
Oncology Center of Excellence
Oncology Center of Excellence works specifically with drugs, devices and biologics for the treatment of cancer.
Center for Tobacco Products (CTP)
Center for Tobacco Products (CTP) reviews premarket applications for tobacco products, oversees the implementation of warning labels and enforces restrictions on promotion and advertising.
Office of Special Medical Programs
Office of Special Medical Programs works with all FDA departments for special programs and initiatives that are clinical, scientific or regulatory in nature. It also leads the Advisory Committee Oversight and Management Staff.
Center for Drug Evaluation and Research (CDER)
Center for Drug Evaluation and Research (CDER) regulates prescription and over-the-counter drugs. Generic drugs and biological therapies are also included in this group. In addition to these, the center also oversees consumer products with ingredients considered a drug such as dandruff shampoo, antiperspirants and fluoride toothpastes.
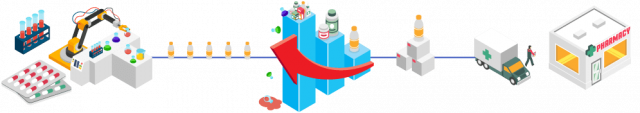
How the FDA Regulates and Approves Drugs
CDER is the largest of the FDA’s six centers and deals with all prescription and over-the-counter drugs. When drug companies need new drug approval, they submit their applications to CDER. The center does not conduct its own tests on drugs. Instead it relies on data and research provided by drug manufacturers.
This center works with drug companies throughout the drug-approval process from the application to the final drug approval. A team of CDER scientists, physicians, statisticians, chemists and pharmacologists review the data and propose labeling for pharmaceutical products.
- Drug company develops drug and conducts animal testing
- Drug company sends an investigational new drug application (IND) to the FDA with a plan for human clinical trials
- Drug manufacturer conducts Phase I, II, and III clinical trials on humans
- Drug company fills out a formal new drug application (NDA) for marketing approval
- FDA reviews clinical trial data for drug safety and effectiveness
- FDA reviews proposed drugs label and inspects manufacturing facilities
- FDA will either approve or deny the drug
Fast Track Programs
The FDA approves more drugs faster than its counterparts in Europe and other countries. In order to keep up with the demand for new treatments, Congress passed the Prescription Drug User Fee Act (PDUFA) in 1992. This law allowed drugs that meet needs for serious or life-threatening conditions to be approved more quickly. Under the PDUFA, the FDA created a number of fast-track programs to facilitate faster approval.
- Fast-Track Designation
- Allows priority review of drugs for unmet medical needs and serious conditions.
- Accelerated Approval
- The program is intended to provide patients with serious diseases more rapid access to promising therapies. Indeed, it allows for earlier approval of these therapies based on a surrogate endpoint. A surrogate endpoint is defined by FDA as “a marker, such as a laboratory measurement, radiographic image, physical sign or other measure that is thought to predict clinical benefit, but is not itself a measure of clinical benefit.” It is used when the clinical outcomes might take a very long time to study. Therefore, the use of a surrogate endpoint can considerably shorten the time required prior to receiving FDA approval.
- Breakthrough Therapy Designation
- Preliminary clinical trials should show that the therapy offers substantial treatment advantages (safer or more effective) over existing options for patients with serious or life-threatening diseases.
- Priority Review Designation
- A priority review designation means that the FDA’s goal is to take action on an application within six months (compared to 10 months under standard review). This is for drugs that are very effective at treating, diagnosing or preventing a condition. Priority review drugs may also work better with fewer side effects than drugs already on the market and treat a new population, such as children or the elderly.
Online Pharmacies and Fake Medications
Online pharmacies are companies that sell drugs on the Internet and sends the orders to customers through the mail or shipping companies. CDER launched a campaign to promote awareness about online pharmacies. Because the FDA does not regulate these products, there is no guarantee of safety. The FDA warns that these drugs may be contaminated, counterfeit, expired or have other quality issues.
These pharmacies may also collect personal and financial information, run internet scams or infect computers with viruses.
In October 2012, the CDER worked with more than 100 other countries to shut down more than 18,000 illegal pharmacy websites.

“The global effort, called Operation Pangea V, took place Sept. 25 through Oct. 2, 2012. By the end of the week, regulatory agencies seized 3.7 million doses of fake medicines worth $10.5 million and 79 people were arrested, Reuters reported.”

Interpol, the World Customs Organization, the Permanent Forum of International Pharmaceutical Crime, the Heads of Medicines Agencies Working Group of Enforcement Officers, Pharmaceutical Security Institute and Europol directed Operation Pangea V.
The FDA took action against 4,100 websites. Three main companies — CanadaDrugs.com, Eyal Bar Oz and Arkadiy Kisin/White Forest Solutions — were linked to most of the 4,100 illegal pharmacies, according to Bloomberg Businessweek.
They received warning letters from the FDA, stating that their websites were offering unapproved drugs to U.S. consumers. The agency gave the companies 10 days to respond to the allegations. The FDA also notified internet service providers that the websites were selling illegal products.
- Viagra, Levitra and Cialis, erectile dysfunction drugs
- Norplant, a contraceptive
- Unapproved generic version of influenza treatment Tamiflu
- Unapproved antibiotic Baycip TZ
- Stomach disorder drugs
Medical Device Regulation and Approval
The Center for Devices and Radiological Health (CDRH), another branch of the FDA, approves all medical devices sold in the United States. It also oversees how the devices are manufactured and monitors their safety. Depending on the classification of the device — Class I, II, or III — the manufacturer will apply for FDA clearance through two general methods: the 510(k) premarket notification or the premarket approval (PMA).
Class I devices are low-risk devices such as dental floss. Class II devices are higher risk and require more regulatory controls. Class III devices usually sustain or support life, are implanted, or present potential risk of illness or injury. Examples of Class III devices include implantable pacemakers and defibrillators.
510(k) Premarket Notification
Under the 510(k) premarket notification process, before a manufacturer can market a medical device of any class in the United States, they must demonstrate to the FDA that it is substantially equivalent (as safe and effective) to a device already on the market. If FDA rules the device is “substantially equivalent,” the manufacturer can market the device.
Premarket Approval (PMA)
Premarket approval (PMA) is the FDA process of review to evaluate the safety and effectiveness of Class III medical devices with rigorous testing.
How FDA Conducts Recalls
A recall is the removal or correction of a product due to problems that are in violation of the law and therefore subject to legal action by the FDA. Recalls can be conducted on a firm’s own initiative, by FDA request, or by FDA order. Although the FDA has the authority to recall biologics (products made of human cells or tissues like vaccines), devices and infant formulas, it does not have the authority to order or mandate a drug recall.
“The number of FDA-approved drug recalls has steadily continued to increase. In 2015, there were more than 4,600 drug and device recalls, and 405 of these products had the potential to cause serious harm or death.”
In the case of medical devices, the recalls are usually performed voluntarily by the manufacturer. In rare cases where the manufacturer or importer fails to recall a device that is a risk to health, the FDA may issue an order to recall the device. Manufacturers may send letters to doctors and physicians notifying them, but patients do not receive letters.
Before the FDA decides to send a recall request to a manufacturer, it considers several factors and a committee of experts weighs available safety and efficacy data.
The committee classifies the recall as Class I, II, or III, with I being the most serious. Class I recalled products can lead to serious injury or death.
How FDA is Funded
The FDA’s funding for drug review is a constant source of controversy. Congress passed the Prescription Drug User Fee Act (PDUFA) in 1992. The PDUFA allowed the FDA to collect fees from drug companies to speed up approvals. Currently, about two-thirds of drug-approval funding comes from pharmaceutical companies.
In 2015, FDA spent about $1.1 billion on the review of prescription drug applications, according to the Project on Government Oversight. Only 29 percent of that money came from Congress. This means taxpayers funded $331.6 million while drug companies provided the lion’s share at $769.1 million.
Although that lessens the burden on taxpayers, some consumer watchdogs say the costs could be passed on to consumers through higher drug prices.
More importantly, the FDA may approve products faster under the influence of Big Pharma at the expense of public safety, said Michael A. Carome, director of Public Citizen’s Health Research Group.
Adverse Event Reporting
After a drug, medical device or vaccine hits the market, the FDA depends on voluntary reporting of manufacturers, hospitals, doctors and patients to track side effects or complications stemming from these products. If a manufacturer receives an adverse event report, it is required to pass this information on to the FDA.
Regulatory actions include: updating safety labels, restricting the use of a drug or device, communicating safety information to the public or removing a product from the market. The FDA rarely requests a product withdrawal.
FAERS, MAUDE and VAERS data does have limitations, according to the FDA. For instance, because reporting is voluntary, there may be more adverse events than the agency is aware of. There is also no guarantee the side effect is directly related to the drug, device or vaccine.
FDA and Clinical Trials
While the FDA does not conduct clinical trials, it has the responsibility of protecting clinical trial participants and making sure data is available to the public on ClinicalTrials.gov. The FDA’s Office of Good Clinical Practice oversees the ethical treatment of participants in clinical trials.
The agency also oversees and regulates clinical-trial protocols called Good Clinical Practice (GCP). Researchers for drug companies and others conducting clinical trials refer to these protocols when designing each phase of their clinical trials, particularly if these trials are funded by the National Institutes of Health.
In January 2017, the NIH and FDA required all NIH-funded clinical trial staff be trained in GCP. These principles help assure the safety, integrity, and quality of clinical trials, according to the FDA.
FDA Scandals and Controversy
The FDA is the most powerful agency of its kind in the world, according to Daniel Carpenter, author of Reputation and Power: Organizational Image and Pharmaceutical Regulation at the FDA. It shapes the drug and device industry with its decisions, and many other countries follow the agency’s lead.
Unfortunately, the FDA has had its share of controversy involving corruption and cover-ups.
Employees Pressured to Approve Devices
Some workers in the medical-device review department of the U.S. Food and Drug Administration (FDA) say they feel pressured to approve devices that they are not sure are safe, according to a new survey reported in the Minneapolis Star Tribune.
Almost 1,000 FDA employees — 17 percent of the total solicited — took the survey. Of those, 158 survey participants worked in the center for devices. About 25 percent said they felt pressured to approve products “despite reservations about the safety, efficacy or quality of the product.”
The Vioxx Scandal
In 2000, one year after the FDA approved Vioxx, a clinical trial identified numerous heart risks associated with the drug, but drug maker Merck downplayed Vioxx’s dangers. In a congressional investigation into how Merck and the FDA handled the Vioxx recall, documents revealed that Merck knew about the severe health complications but heavily marketed the drug anyway.
Further investigation revealed that the FDA may have acted unethically as well. David Graham, an FDA researcher, testified that the agency subjected him to ostracism, veiled threats and intimidation when he attempted to publish findings that linked Vioxx to 27,000 heart attacks or sudden deaths from 1999 to 2003. In emails Graham produced, his superiors suggested watering down the study’s conclusions.
FDA Hides Evidence of Fraud in Clinical Trials
When the FDA finds evidence that a drug company falsifies information in clinical trial data, it often doesn’t report it, according to a study by Charles Seife, a professor at New York University. The study published in JAMA Internal Medicine in 2015 looked at publicly available FDA inspection documents from January 1998 through September 2013.
Researchers found 57 published clinical trials where the FDA found significant problems but failed to publish these issues or issue corrections.
- 22 Trials
- Had false information
- 14 Trials
- Had problems with adverse events reporting
- 42 Trials
- Had protocol violations
- 35 Trials
- Had inaccurate or inadequate record keeping
- 30 Trials
- Failed to protect patient safety or had issues with informed consent
- 20 Trials
- Had unspecified violations
FDA Milestones & History
Although the agency has faced criticisms, it has a history of protecting the public from health disasters.
For example, in 1937 after a drug called Elixir Sulfanilamide killed more than 100 people, the FDA sent out agents to physically pull the drug off shelves and advise physicians to stop prescribing it, preventing more loss of life. This led Congress to give FDA more power to regulate drugs.
In the 1960s, an FDA medical officer named Dr. Frances Kelsey stopped the sale of a sedative called thalidomide in the U.S. after she discovered it had not been properly tested, she did not approve the drug for sale. As a result, she prevented birth defects in the U.S. that happened to thousands of children in other countries.
The FDA’s actions led to the evolution of drug and device regulation laws in the U.S. granting it more regulatory power.
-
1862
President Lincoln appoints a chemist, Charles M. Wetherill, to serve in the newly-established Department of Agriculture. This leads to the creation of the Bureau of Chemistry, predecessor to the Food and Drug Administration.
-
1906
Congress passes the Food and Drugs Act, which prohibits misbranded drugs, food and drinks in interstate commerce.
-
1914
The Harrison Narcotic Act requires prescriptions for products containing certain amounts of narcotics. It also increases recordkeeping for doctors who provide narcotics.
-
1927
The Bureau of Chemistry is divided into two entities: the Food, Drug and Insecticide Administration and the Bureau of Chemistry and Soils.
-
1930
An agricultural appropriations act shortens the name of the Food, Drug and Insecticide Administration to the Food and Drug Administration (FDA).
-
1938
Congress passes the Federal Food, Drug and Cosmetic (FDC )Act, establishing a new system of drug regulation that requires premarket safety testing for drugs.
-
1966
The Fair Packaging and Labeling Act requires honest labeling for food, drugs, cosmetics and medical devices, with provisions enforced by the FDA.
-
1970
The FDA requires the first patient package insert for oral contraceptives, informing patients of specific risks and benefits.
-
1972
The Over-the-Counter Drug Review process is established to improve the safety, effectiveness and accurate labeling of drugs sold without a prescription.
-
1976
The Medical Device Amendments passes, allowing the FDA to ensure the safety of medical devices and diagnostic products. Some products require FDA pre-market approval, while others must pass pre-marketing performance standards.
-
1988
The Food and Drug Administration Act officially establishes the FDA as an agency of the U.S. Department of Health and Human Services.
-
1990
The Safe Medical Devices Act passes, requiring hospitals and other facilities that use medical devices to report to the FDA any devices that may have contributed to the injury, serious illness or death of a patient. The act also requires manufacturers to conduct post-marketing surveillance on high-risk implanted devices and authorizes the FDA to order medical device recalls.
-
1992
Congress passes the Prescription Drug User Fee Act, which allows the FDA to collect fees from drug manufacturers to fund the approval of new drugs.
-
1993
Several adverse event reporting systems are combined to form MedWatch, a system for the voluntary reporting of medical-product complications by health professionals.
-
1997
The Food and Drug Administration Modernization Act introduces the most dramatic reform to FDA policy since the FDC Act of 1938. It includes measures to accelerate medical device reviews and regulates advertising of unapproved uses for approved drugs and devices.
-
2005
The FDA announces the formation of the Drug Safety Board. The board includes representatives from the National Institutes of Health, the Veterans Administration and FDA staff, who advise the FDA on drug safety issues and communication with patients and health care providers.
-
2009
President Obama signed the Family Smoking Prevention and Tobacco Control Act. The act gave the FDA authority to regulate tobacco products and it established the Center for Tobacco Products.
-
2011
FDA Food Safety Modernization Act (FSMA) provided FDA with new enforcement authorities for food safety.
-
2012
Food and Drug Administration Safety and Innovation Act (FDA SIA) expands FDA authority to collect user fees from the industry to fund more reviews of drugs and devices. Congress enacted the 2013 Drug Quality and Security Act (DQSA) allowing FDA regulatory oversight over compounded drugs.
-
2013
In July 2013, the FDA proposed that each medical device would carry a unique numeric or alphanumeric code called a unique device identification number. The Pandemic and All-Hazards Preparedness Reauthorization Act (PAHPRA) established and reauthorized certain programs under the Public Health Service Act and the Food, Drug, and Cosmetic Act for all-hazards preparedness and response.
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.




