
Most Americans know someone who has diabetes. In fact, the prevalence of the disease is growing in the U.S. More than 29 million people in the country are living with diabetes, and 8.1 million people don’t know they have the disease.
It’s expensive too. Medical treatment and lost wages for people diagnosed with diabetes costs $245 billion annually. About 86 million people have pre-diabetes, according to the latest numbers from the Centers for Disease Control and Prevention — 9 out of 10 people don’t know they are at risk.
Prescription drug prices in the U.S. have been rising for several years. Some drugs in 2022 increased by more than $20,000 or 500%. Between July 2021 and July 2022, there were 1,216 products whose price increases exceeded the inflation rate of 8.5% for that period. The average price increase for these drugs was 31.6%.
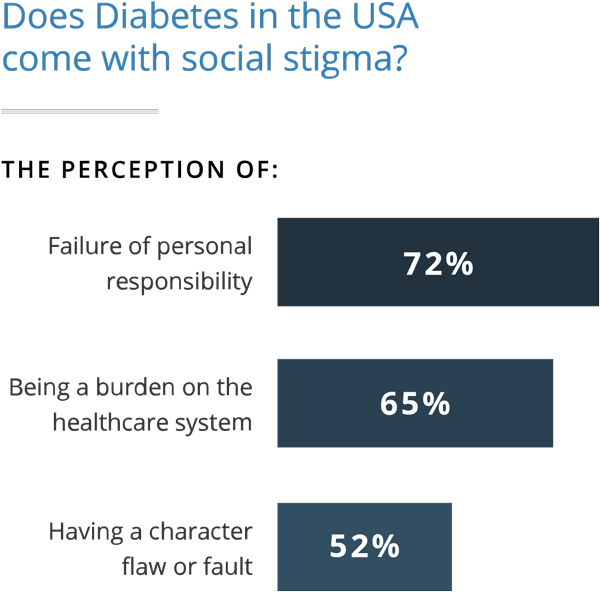
But these figures only tell part of the story. Behind the stats are real people, and the stigma attached to the disease is one of the least known and discussed complications of diabetes. The diabetes blame and shame game is real, and it has a negative impact on self-care, mental health and social life.
Editors carefully fact-check all Drugwatch.com content for accuracy and quality.
Drugwatch.com has a stringent fact-checking process. It starts with our strict sourcing guidelines.
We only gather information from credible sources. This includes peer-reviewed medical journals, reputable media outlets, government reports, court records and interviews with qualified experts.
“Many people with Type 2 diabetes are accused of causing their disease. That is not only unfair, it is incorrect.”
To the majority without the disease, people with diabetes are presented as overweight, lazy and guilty of bringing the disease upon themselves — often illustrated by faceless overweight people in reports on network news. On social media, images of large amounts of sweets often accompany the word “diabetes.”

People with diabetes are those people who have to prick their fingers, inject themselves with insulin or drag around an insulin pump or a bag of medications. If they just got off the couch and stopped eating too much sugar, they would never have gotten the disease to begin with, right?
Wrong.
“Diabetes is a complex disease,” diabetes educator Janis Roszler told Drugwatch. “For example, not everyone who is overweight develops it, and many who have Type 2 are thin.”
While being overweight is a known risk factor Type 2 diabetes, those who have a family history of the disease or had it while pregnant are also at risk, regardless of weight. And Type 1 is actually an immune disorder that occurs when the body destroys its own insulin-producing cells.
These are just a few myths about the disease that people with diabetes face on a daily basis. According to Roszler, there are people with diabetes who “feel they are damaged in some way.”
Through education and developing support and coping mechanisms, people with diabetes can overcome it — and hopefully, understanding will also lead to more compassion.
Diabetes Stigma: The Blame and Shame Game
Fat, obese, overweight, big fat pig, lazy, slothful, couch potato, over-eater and glutton — these were a few of the negative stereotypes associated with people with Type 2 diabetes, according to participants in a study conducted by Jessica L. Browne and colleagues published in 2013 in BMJ.
“Once again, these stereotypes reflected the idea that you brought it on yourself,” Browne and colleagues wrote. “Less frequently reported were stereotypes of people with T2DM being poor people, not terribly intelligent, as well as being a shocking person or bad personand injecting insulin.”
“I think the stigma is that it's a lifestyle disease. That somehow you've been lazy, and you've allowed this to happen to yourself.”
Few other diseases carry the social stigma of diabetes. For example, most people never blame breast cancer patients for getting cancer. There are a number of positive, empowering campaigns for cures and awareness. Supporters wear pink and celebrate survivors. According to the American Cancer Society, the 5-year survival rate for women with breast cancer that has not spread is nearly 100 percent.
“Many cancers are curable. There is no current cure for diabetes that is available to the general public,” said Roszler. “Those who have it must monitor what they eat, check their blood, take their medication (if needed) and stay physically active to stay healthy.”
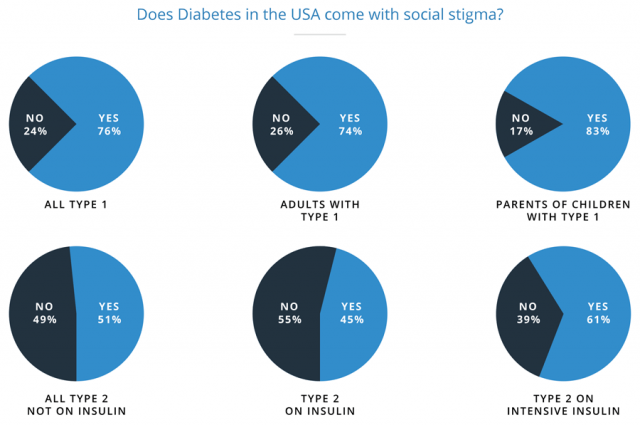
But in contrast to other diseases, the public is less accepting or encouraging of people living with diabetes. In fact, studies show more than half of Americans with Type 1 and 2 diabetes feel others blame them for their disease. A staggering 83 percent of parents of children with Type 1 feel the public blames them for causing their child’s disease.
For example, a common practice among health care providers and people without diabetes is to call someone with the disease a “diabetic.” Karen Kemmis, a diabetes educator with SUNY Upstate Medical University in Syracuse, New York, says this labeling is a “huge pet peeve” of hers and many educators and people with diabetes. According to Kemmis, this depersonalization contributes to the stigma.

“We don’t call someone who has cancer a canceric and shouldn’t call someone with COPD a COPDer,” Kemmis told Drugwatch. “But, somehow, it seems acceptable to many to call someone a diabetic. No, they have diabetes. We should use person-first language rather than label someone by a disease.”
The burden of the disease on those affected can be considerable. Experts call it diabetes distress, a mixture of depression, anxiety and stress. Research conducted by Dr. Lawrence Fisher, professor at the Diabetes Center of the University of California in San Francisco, found about half of people with diabetes will experience it.

Fisher found one of the contributing factors to the distress is “social burden.” The stigma attached to the disease takes its toll, Fisher told Diabetes Forecast. Researchers found suffering from distress and stigma-induced shame leads to poor self-care and worse health outcomes.
“Elevations in depressive symptoms and/or diabetes-related distress should be recognized as a predictor of problems with medication adherence in adults with type 2 diabetes,” Dr. Jeffrey S. Gonzalez associate professor of psychology at the Ferkauf Graduate School of Psychology of Yeshiva University, New York, told Endocrine Today.
The more intense the therapy, the more intense the stigma, Alexandra E. Folias and colleagues of dQ&A Market Research found. For instance, 43 percent of those with higher A1C levels who injected insulin or used a pump felt stigmatized, versus 25 percent of those with lower A1C levels.
The damaging stigma surrounding the disease comes from a handful of myths.
“I find a lot of people, they like to think of you as being the culprit. In fact I actually had one person say, 'Well, you've dug your grave with your own teeth.”
Myth: People with Type 2 Diabetes Caused Their Disease
One of the strongest and most hurtful myths is that people with Type 2 diabetes wished it upon themselves and willingly gave themselves the disease. Kemmis has seen firsthand how the blame negatively impacts people with diabetes.
“I guess it is similar to people that have a disease that is related to cigarette smoking. It is their fault,” Kemmis told Drugwatch. “It can increase guilt and shame and could contribute to challenges in self-management. It is so important that people understand that family history and many other factors are involved in the onset of diabetes.”
For instance, another factor that increases the risk of developing Type 2 is gestational diabetes. Gestational diabetes occurs when pregnancy hormones decrease insulin sensitivity.
After her Type 2 diagnosis, Sue Rericha — a 45-year-old elementary school teacher — had a friend tell her, “Oh, it runs in our family too, but we’re watching our weight so we won’t get it.” She told Diabetes Forecast that she felt her friend was calling her “fat” even though she had a normal body mass index and Type 2 ran in her family. She also had gestational diabetes during pregnancy five times.
Myth: Eating too Much Sugar Causes Diabetes
“There’s always someone who makes a comment, 'It’s just because you’re fat and lazy. You just need to stop eating so much.' It’s very frustrating, and usually I just have to step back.”
Another popular misconception is that eating sugar or carbs causes diabetes. While doctors are still learning about Type 1 and 2 diabetes, according to the Joslin Diabetes Center, “What is known is that eating too many sweets doesn’t cause diabetes!”
This myth also leads to what Kemmis calls the “diabetes police.” The police are usually family members and friends who watch everything a person with diabetes does — especially sugary food intake.

“You shouldn’t have that dessert or drink that regular soda or eat that pasta. You should exercise and stop eating carbs, [according to the diabetes police],” Kemmis told Drugwatch. “Another issue is people blaming parents for ‘giving’ their child Type 1 diabetes because they gave them too much candy/sugar. This has nothing to do with it!”
There is no specific diabetes diet for people with Type 2. Experts say each person is different, and eating sweets is not necessarily off the menu after diagnosis. Each individual should work with a care team that can create a meal plan that works for them.
Myth: Type 2 Diabetes Can Be Permanently Cured
“The good news for a type 1 and type 2 patient is that if insulin, medication, weight loss, physical activity and changes in eating result in normal blood glucose, that means their diabetes is well controlled and their risk of developing diabetes complications is much lower. But it doesn't mean that their diabetes has gone away.”
Because of misconceptions about how Type 2 diabetes develops, the myth spread that an adjustment to diet and activity, just getting off the couch and eating less, can cure it. But, the truth is people with Type 2 have to live with it for the rest of their lives.
Type 2 diabetes is a progressive disease, and sometimes people might need more medications than they did at the time of diagnosis. This could mean progressing from oral medicines to injecting insulin. Some patients may feel like failures when this happens.
Sources of Stigma
“That’s just the nature of diabetes. Sometimes you need medicine to reverse things that aren’t working metabolically in your body.”
There are several sources of diabetes stigma. These messages can affect people with and without diabetes, and many have a negative effect regardless of intent. Browne and colleagues identified the media, healthcare professionals and family and friends as the main sources.
Because of the stigma, people newly diagnosed with diabetes may even keep it a secret for fear of judgement. They fear discrimination at work and the sense of blame they may get from others. For example, one study participant said she felt the need to hide it because she had a high-ranking position at her company.
Stereotypes can even lead to discrimination and restricted opportunities, though U.S. law lists diabetes as a disability and protects individuals from discrimination. Negative perceptions of the disease — particularly if an individual is overweight — may affect job opportunities and relationships.
The Media
Media is even more prevalent than ever, and people can watch TV or look online to see presentations of people with diabetes — particularly Type 2 diabetes.
As our media shifts to digital content, the internet is a growing source of stigma. Mike Durbin is a 31-year-old health blogger diagnosed with Type 2 diabetes and congestive heart failure in 2008. In an interview with Diabetes Forecast, he spoke about reader comments on his 2011 USA Today profile.
“Some of the [online comments] were: ‘If this guy would just get off his [couch] and do something, try exercising, try eating better, [he wouldn’t have diabetes]’ — most of the typical comments that you hear toward people with type 2,” he said. “I’ve gotten to where I really don’t take much of that to heart. It would really just eat you alive if you did.”
Browne’s research points to two views expressed in the media: Type 2 is a lifestyle disease, and emphasis on being overweight and physically inactive reinforced blaming attitudes. People with Type 2 diabetes also felt media often used scare tactics and sensationalism to describe the “diabetes epidemic.” Few stories or features focus on people who successfully manage the disease.
Healthcare Professionals
Healthcare professionals are also a source of negative feelings and stigma. Participants in Browne’s study reported their doctors focused on what patients did “wrong.” They wanted more encouraging behavior and helpful tips on how to improve. Patients instead reported feeling discouraged and judged.
“The reason is clear: Type 2 diabetics tend to be obese, and we still think of obesity as a self-created illness, caused by too much eating and too little exercise,” Dr. Sanjay Gupta wrote in Everyday Health. “Even some doctors will admit they are less sympathetic to their diabetic patients.”
“The dietician was awful... she asked me if I exercise, and I said 'I do the gym twice a week and I have consistently since November.' 'That's not enough, you need to go five times a week.' This makes me really angry.”
In a story about stigma, Gupta interviewed Dr. Peter Attia, a physician who judged his patients with Type 2 because they were overweight until he had his own run-in with prediabetes.
“[My patient] was in the emergency room for a condition I considered completely preventable,” Attia told Gupta. “She did in fact sense this was a physician who was judging her.”
“There’s no good news stories about type 2 diabetes. Perhaps there should be. Perhaps it should be 'it isn’t necessarily a death sentence.'”
But, while he judged his patients, Attia was borderline obese despite daily exercise and healthy eating. Then he found out he had prediabetes. Now he speaks about shedding the stigma of obesity and diabetes.
Another misconception that may spread among healthcare practitioners is that people with Type 2 diabetes need to lose large numbers of weight to make a difference. The information may be discouraging to people with diabetes.
“Many people think they need to lose 50 or 100 pounds when studies show that diabetes management can change with a modest 5-10 pound weight loss and moderate exercise of 30 minutes/5 days per week,” Karen Kemmis told Drugwatch.
Friends, Family and Colleagues
“I'd love it if you offer me what [food] you're handing around and I can say 'yes' or 'no thanks,' that would be nice really. That makes me feel excluded.”
Despite the best intentions, family and friends may be hurtful and judgmental. People with Type 2 described the behavior as “unhelpful, annoying or discouraging” and found it “hurtful, judgmental and interfering.”
“We talk about the ‘diabetes police’ who might be friends or family that watch a person with diabetes and tell them what they should and shouldn’t do,” said Kemmis. “No one likes to be told what to do or eat. It’s the idea that it is the person’s own fault for getting themselves into this mess.”
Significant Others and Dating
Type 2 diabetes stigma also extends to social life, particularly in intimate situations with spouses or even dating. When it comes to intimacy with a spouse or partner, the fear can be crippling.
Diabetes educator Janis Roszler is also a marriage and family therapist, and she has seen the stigma affect marriages and relationships.
“When I first got it I wouldn't tell anybody. I didn't even tell my husband. I told nobody. I actually felt so ashamed to have diabetes. I felt completely ashamed of myself.”
“About half of all men and women with diabetes develop some form of sexual complication,” Roszler told Drugwatch. “Men who struggle with their diabetes management are at an increased risk of developing erectile dysfunction. Women may have vaginal dryness, pain during intercourse, arousal and orgasm challenges, and an increased incidence of urinary tract infections.”
Sexual dysfunction of any kind already comes with a hefty dose of shame, and according to Roszler, diabetes-related dysfunction adds more shame to it.
“They worry that others may not want to date someone who lives with a chronic disease that requires so much daily attention,” she said. “I’ve interviewed many people with diabetes who struggled to find a positive way to tell people they date about their diabetes.”
While it can be difficult to overcome, Roszler offers some suggestions to lessen the anger and frustration that can come with diabetes-related complications.
“Give ‘diabetes’ a name, and treat it like a totally separate entity,” she said. “I know of a couple who named the husband’s diabetes ‘George.’ When the husband started to feel his blood sugar drop during sexual activity, they blamed ‘George’ for making trouble, not the husband.”
Demystifying Diabetes and Dispelling Myths
“Many of my patients are frustrated because the general public doesn't understand what they go through each day. Diabetes affects every area of a person's life. It isn't possible to take a vacation from it.”
Even though about a third of Americans have diabetes or prediabetes, there are still misconceptions about the disease. Education is one of the ways to dispel these myths. So, here are the diabetes basics. People can get diabetes at any age. Men and women can develop the disease — though men are more likely to develop it. According to the American Diabetes Association, the disease is the seventh leading cause of death in the U.S.
Currently, there is no cure for diabetes though people can manage it through lifestyle changes and medical treatment. There is more than one type of diabetes, and each type has its own risk factors.
Symptoms of Diabetes
According to the National Institutes of Health, there are a few key symptoms of diabetes, though some people might not have any symptoms.
- Extreme thirst
- Blurry eyesight
- Dry, itchy skin
- Feeling very hungry
- Fatigue
- Feelings of pins and needles in your feet
- Losing feeling in your feet
- Losing weight without trying
- Sores that heal slowly
- Urinating often
Types of Diabetes and Treatment Options
There are three main types of diabetes: Type 1, Type 2 and Gestational. Doctors develop treatment plans based on which type a person has.

Type 1
This type of diabetes occurs when the body’s own immune system attacks and kills the cells that produce insulin. This stops the body from making enough insulin to manage blood sugar. This is the rarest form of diabetes and makes up about 5 to 10 percent of all diagnosed cases in the U.S. Because this type develops most often in children and young people, doctors previously called it juvenile diabetes. But, adults can also develop Type 1 diabetes.
Treatment for Type 1 includes:
- Insulin shots
- Oral medications
- Watching diet and being physically active
- Controlling blood pressure and cholesterol

Type 2
The majority of all diabetes cases in the U.S. — 90 to 95 percent — are Type 2. This type occurs when the body doesn’t produce enough insulin or loses insulin sensitivity. Because it most often affects adults, doctors used to refer to it as “adult-onset” diabetes.
Treatment for Type 2 includes:
- Oral medications
- Insulin shots
- Diet and exercise
- Keeping a healthy weight
- Managing blood pressure and cholesterol

Gestational
This type of diabetes affects pregnant women. According to the American Diabetes Association, 9.2 percent of pregnant women may be affected. While doctors don’t know the exact cause, they think gestational diabetes occurs when hormones released during pregnancy affect insulin resistance.
If left untreated, gestational diabetes can lead to babies with breathing problems and a higher risk for obesity and Type 2 diabetes later in life. Diet and exercise during pregnancy often work to keep gestational diabetes in check. It typically resolves after pregnancy, but mothers with gestational diabetes are at risk of developing Type 2.
Diagnosing Diabetes
Doctors use three main tests to diagnose diabetes: A1C, fasting plasma glucose (FPG) and oral glucose tolerance test (OGTT). Each test has normal, pre-diabetes and diabetes levels.
-
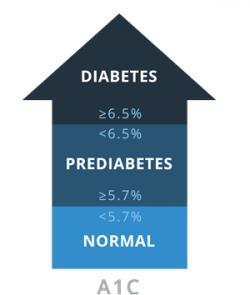 A1CMeasures average blood glucose over the course of 2-3 months.
A1CMeasures average blood glucose over the course of 2-3 months. -
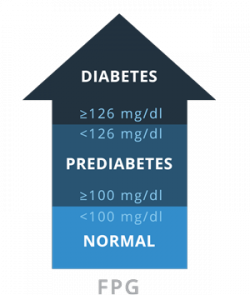 FPGMeasure levels of fasting blood sugar. Patients should be fasting for at least 8 hours prior to the test.
FPGMeasure levels of fasting blood sugar. Patients should be fasting for at least 8 hours prior to the test. -
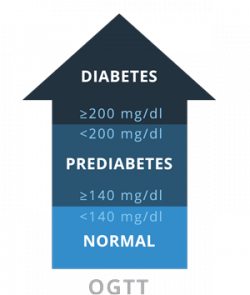 OGTTThis test measures blood glucose before and 2 hours after drinking a special drink with sugar.
OGTTThis test measures blood glucose before and 2 hours after drinking a special drink with sugar.
Type 2 Medications and Possible Side Effects
Another unfortunate risk of diabetes comes from serious side effects that may occur because of medications. While sometimes medication is necessary to help maintain good health in people with diabetes, and many are effective at controlling excess blood sugar, everyone is different and some may react poorly to a particular drug. Studies also link some drugs to more serious side effects.
People with diabetes should research each drug and have conversations with their doctor about the risks and benefits. There are several options to treat Type 2 diabetes, and some drugs are older than others.
Sodium-glucose co-transporter 2 (SGLT2) Inhibitors
Sodium-glucose co-transporter 2 (SGLT2) Inhibitors are some of the newest drugs available, and the U.S. Food and Drug Administration approved the first drug in the class, Invokana, in 2013. These drugs work by stopping the kidneys from reabsorbing sugar into the blood. The excess glucose leaves the body through the urine. The U.S. Food and Drug Administration and studies link these drugs to serious and life-threatening side effects. The FDA released its first warning in 2015.
- Invokana (canagliflozin)
- Farxiga (dapagliflozin)
- Jardiance (empagliflozin)
Serious side effects may include:
- Urinary tract infections that lead to blood infections
- kidney injury
- diabetic ketoacidosis (DKA)
DPP-4 Inhibitors
These drugs work by stopping an enzyme that prevents the pancreas from making more insulin. This means more insulin circulates in the blood longer, helping to metabolize excess sugar. Studies and the FDA link these drugs to some serious side effects. The FDA approved Januvia, the first DPP-4, in 2006.
- Januvia (sitagliptin)
- Onglyza (saxagliptin)
- Trajenta (linagliptin)
Serious side effects may include:
- Pancreatitis
- Pancreatic cancer
- Heart failure
- Severe joint pain
Thiazolidinediones (TZDs)
These drugs work by decreasing insulin resistance and helping the body’s cells become more sensitive to insulin. The first TZDs arrived on the market in the late 1990’s. This is one of the most problematic classes of Type 2 diabetes drugs, and studies linked them to bladder cancer and heart problems. Drug makers paid billions in settlements to people who said the drugs caused bladder cancer and fatal heart attacks.
Brands of TZDs Include:
Actos (pioglitazone), Avandia (rosiglitazone) and Rezulin (troglitazone) — Rezulin was pulled from the market because of hepatitis concerns.
Tips for Overcoming Diabetes Stigma
Diabetes educators agree that education and awareness are the best ways to fight stigma. The more information people without diabetes have, the less likely they are to incorrectly pass judgement.
“Helping the public to increase awareness of the emotional components of diabetes would be good,” Karen Kemmis told Drugwatch. “It isn’t something that people will likely change with scare tactics. It is really important for people to know that there are many factors to getting diabetes, some that are changeable and others that aren’t.”
People with diabetes also deal with guilt and self-stigma. Janis Roszler advocates discussing challenging issues with a support group, and if necessary, seeking out a mental health professional.
“For those who continue to struggle, I suggest they meet with a mental health professional who can help them perceive themselves and their diabetes in a more positive way,” Roszler said. “How a person perceives him/herself makes all the difference. A good therapist can help with that.”
Health care providers can help their patients make meaningful strides, too. Studies show empathy from providers can break down stigma.
“It is really important for people to know that there are many factors to getting diabetes, some that are changeable and others that aren’t.”
For example, at the 2015 American Diabetes Association Scientific Sessions Boehringer Ingelheim and Eli Lilly conducted an experiment. They collected data on the lifestyle choices of attendees. Researchers found researchers, clinicians and other industry professionals chose brownies over veggies and 84 percent chose escalators over stairs. It showed even professionals slip up on the guidelines they give their patients. Study researchers suggested that more empathy from providers would improve their patient’s care and lead to more positive health care.
Above all, people with diabetes should take one step at a time and be kind to themselves.
“It is good for a person to take positive steps, work with a diabetes educator for strategies to successful behavior change, and to try to make positive changes and feel good about them,” said Kemmis. “Trying to be perfect rarely works out. Just focus on small changes to be successful and then move on to the next.”
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.