Arthritis
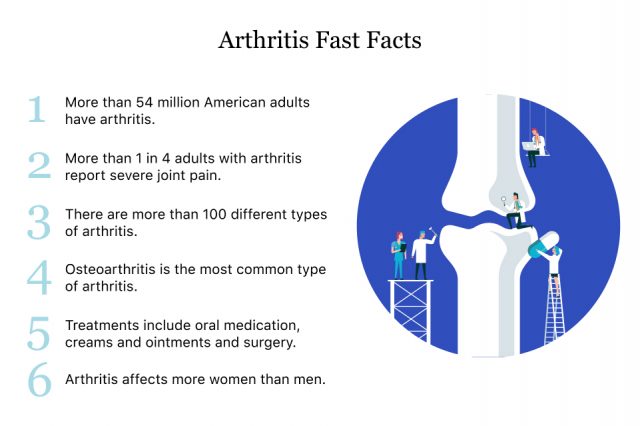
Arthritis is degeneration or inflammation in the joints, and it can affect one or more joints. Out of the more than 100 types of arthritis, osteoarthritis and rheumatoid arthritis are two of the most common. Treatment options include oral medications, creams or ointments and surgery.

More than 54 million American adults have arthritis, according to the Centers for Disease Control and Prevention. By 2040, about 78 million adults will have the disease. It’s a leading cause of work disability, and it costs the healthcare system $140 billion each year.
Arthritis is more common in older people, but it can affect anyone in any age group. In fact, about 300,000 children have juvenile arthritis, according to Cleveland Clinic.
The most common symptoms of arthritis are swelling, pain and stiffness in the joints. For some people, these symptoms interfere with daily activities and decrease mobility.
There is no cure for arthritis, but available treatments focus on reducing pain and increasing mobility. In addition to standard treatments such as medication and surgery, some lifestyle management programs can improve quality of life and improve arthritis symptoms.

Symptoms
Arthritis symptoms range from moderate to severe and may be different depending on the type of arthritis. Some types of arthritis, such as rheumatoid arthritis, can cause severe damage to joints and deform them.
An ache in the joints every now and then doesn’t always mean arthritis. For example, active people may have aches and pains after running or other high-impact activities.
But routine pain and stiffness, especially in a joint, may be an early sign of arthritis. Swelling in the joint, along with pain and discomfort are often the first symptoms, Dr. Uzma Haque, co-director of clinical operations at the Johns Hopkins Arthritis Center in Baltimore, told AARP.
“If you walk a block and consistently have aching in your right knee, but it improves when you sit down, that’s when you should think, ‘Do I need a medical evaluation?’” Haque said.
- Breathing problems
- Weight loss
- Fever
- Trouble moving and getting around
- Itchiness or rash
- Pain
- Redness, swelling or heat in the joints
Types and Causes
There are more than 100 types of arthritis. Three of the most common types are osteoarthritis, rheumatoid arthritis and psoriatic arthritis, according to the National Institute of Arthritis and Musculoskeletal and Skin Diseases.
Researchers don’t know the exact cause of the disease, but each type causes pain and symptoms in different ways. Each type also has different symptoms and potential treatments.
Osteoarthritis (OA)
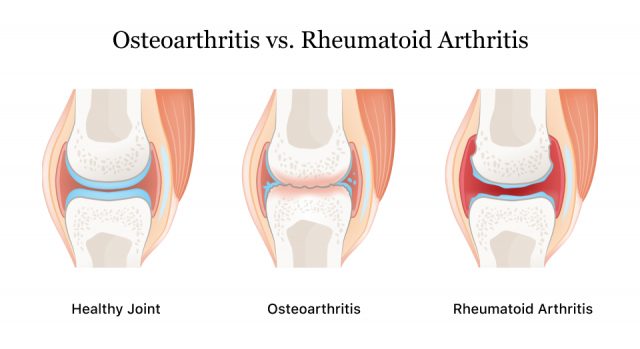
Osteoarthritis causes tissues in the joint to break down over time. It’s the most common type of arthritis and is most likely to affect older people. It affects more than 32.5 million American adults, according to the CDC.
People with OA have pain in the joints, and joints may get stiff after rest for about half an hour. It most often affects the hands, knees, hips, neck and lower back.
Medical providers most commonly treat osteoarthritis with lifestyle changes such as losing weight, adjusting the diet and getting exercise. They may also prescribe medications. If more conservative measures don’t work, a medical provider may recommend surgery.
Rheumatoid Arthritis (RA)
Unlike osteoarthritis, which is caused by age-related wear and tear to joints, rheumatoid arthritis is an autoimmune disease. In RA, the pain, swelling and stiffness are caused by the immune system attacking healthy joint tissues. It involves inflammatory proteins such as tumor necrosis factor-alpha and sulfatase-2. Without treatment, joint damage can be severe and cause deformed fingers and toes.
RA symptoms include joint pain when moving and at rest. Joints will be tender, warm and swollen. People with rheumatoid arthritis may have fevers, feel tired and lose their appetite. In addition to problems with joints, RA can lead to problems with the skin, eyes, heart, lungs, blood and nerves.
Treatments include medications for pain, swelling and slowing joint damage. Doctors may recommend joint replacement surgery in some cases.
Psoriatic Arthritis
Psoriatic arthritis affects joints and areas where skin attaches to bone. Researchers aren’t exactly sure what causes this disease, but it may be related to genes and the environment.
It most often occurs in people with psoriasis, a skin condition where people develop red or white scaly skin patches. Symptoms typically begin between ages 30 and 50, but it can also happen to children. This disease most often affects the lower back, ankles, knees, wrists and outer joints of toes or fingers.
Symptoms include joint stiffness, pain and stiffness in the neck and lower back, tender heels, red and warm joints, thickness or reddening of the skin, pink eye or other infections and sausage-like swelling of fingers or toes.
Medication is the most common treatment.

Risk Factors
While researchers don’t know the exact causes of arthritis, they have identified risk factors that make people more likely to develop the disease.
According to the CDC, some of these factors are non-modifiable, meaning you are born with these factors. Others are modifiable, meaning you can take medications or make lifestyle changes to lower your risk.
- Age
- Risk increases with age.
- Gender
- Most types of arthritis are more common in women.
- Genetics
- People born with certain genes are more likely to develop some types of arthritis.
- Weight
- People who are overweight or obese can make arthritis worse, particularly in the hips and knees. Maintain a healthy weight to avoid putting extra strain on joints.
- Infection
- Infections can affect joints and cause certain types of arthritis. See your doctor if you have red, warm or swollen joints to make sure it’s not an infection.
- Injury to Joints
- Excessive stress on joints or repetitive overuse may cause joint damage and lead to osteoarthritis in that joint. Special exercises for these joints may help prevent injury.
- Your Job
- Some jobs may require repetitive bending or squatting and are associated with knee osteoarthritis. Learn about ways to preserve your joints and be mindful of your physical limitations and abilities.
- Smoking
- Smoking increases a person’s risk for RA and can worsen existing disease. Stop smoking, and get help to quit if you need it.
Comorbidities
Arthritis comorbidities are other diseases that a person with arthritis may also have. Arthritis is more common in people with obesity, diabetes and heart disease.
Because arthritis makes it difficult to be physically active, it may increase a person’s risk of developing these other conditions. Increasing physical activity has benefits for controlling arthritis and these other diseases.
Is Arthritis Hereditary?
It’s likely that genes play a role in a person’s risk for developing arthritis, according Cleveland Clinic rheumatologist Dr. Abrahim Syed. People with family members with arthritis may also be more likely to develop it.
For example, some people with hereditary OA have genetic mutations in genes for collagen — a main component in joint connective tissue. About 40 to 65 percent of osteoarthritis cases have a genetic component, especially in arthritis of the hand or hip.
More than 100 genes could be linked to RA. These genes may make a person more likely to have an immune response to infection, injury or smoking that could lead to RA symptoms.
About 90 percent of people with ankylosing spondylitis — a type of arthritis that affects the spine — carry a gene called HLA-B27. But not everyone with HLA-B27 develops AS.
Diagnosing and Testing for Arthritis
To diagnose arthritis, medical providers will review your medical history, examine your joints, order lab tests and may take a sample of fluid from your joint. Two main types of testing for arthritis are laboratory tests and imaging tests.
Laboratory Tests
Lab tests involve taking a blood or fluid sample and examining it for blood cell count, inflammation and antibodies that may be signs of arthritis. These tests may also determine the type of arthritis a person has.
Antinuclear Antibody
This test checks for antibodies that people with arthritis may produce.
Joint Aspiration (Arthrocentesis)
Doctors will insert a needle into the joint and take a small sample of joint fluid called synovial fluid. Lab workers will examine it for cell counts, synovial fluid crystals and other tests.
Complement Tests
This type of test measures the level of a group of proteins in the blood called complement. This test is useful for diagnosing RA.
Complete Blood Count
This measures white blood cells, red blood cells and platelets. Low levels of blood cells may indicate certain types of arthritis.
C-Reactive Protein
Elevated levels of c-reactive protein may indicate inflammation and could mean a person has arthritis.
Erythrocyte Sedimentation Rate
This test looks at how quickly red blood cells settle to the bottom of a test tube. Elevated rates may indicate inflammation and arthritis.
Hematocrit
This test measure levels of red blood cells. Low levels may indicate arthritis.
Rheumatoid Factor
This test looks for an antibody present in most people with RA.
Urinalysis
Lab technicians will check urine for indications of kidney disease associated with some types of arthritis.
Uric Acid
High levels of uric acid could indicate gout, a type of arthritis.
Imaging Tests
Medical providers use imaging tests to examine the joint for damage. These tests include X-rays, ultrasounds, MRIs and arthroscopy.
MRIs are more detailed than X-rays and can show damage to bone, ligaments, muscles and cartilage.
Arthroscopy is an invasive procedure where a surgeon inserts a thin tube with a lighted camera at the end of it into the joint through a small incision. The camera projects images of the joint onto a screen. The doctor can see arthritic changes to the joint, detect bone disease, detect tumors and determine what is causing inflammation and pain.
Treatment
Depending on the type and severity of arthritis, treatment may involve lifestyle changes, medications and pain-relieving creams or ointments. In severe cases, a doctor may recommend joint replacement surgery.
Medication
There are several medication options for treating arthritis by type of arthritis and severity of symptoms.
Analgesics
These medications help reduce pain, though they don’t reduce inflammation. Some over-the-counter drugs may be sufficient to handle mild to moderate pain, such as Tylenol (acetaminophen).
For more severe pain, doctors may prescribe opioids. These include Ultram (tramadol), OxyContin (oxycodone) or Zohydro ER (hydrocodone). People should be careful with using opioids because they may be habit-forming.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
Like analgesics, NSAIDs are available over-the-counter or by prescription. These medicines reduce pain and inflammation. Over-the-counter NSAIDs include ibuprofen known by brand names such as Advil, Motrin IB and others. Aleve (naproxen) is another popular NSAID sold over the counter.
NSAIDs may increase the risk of heart attack or stroke and cause stomach irritation. An older prescription NSAID called Vioxx (rofecoxib) was pulled off the market in 2004 because of an increased risk of heart attack.
NSAIDs may also come in creams that patients can rub on joints.
Counterirritants
Counterirritants are creams and ointments that contain capsaicin — the chemical that makes peppers hot — or menthol. These creams may help relieve pain.
Disease-Modifying Antirheumatic Drugs (DMARDs)
These drugs are often used to treat RA and work by stopping the immune system from attacking the joints. Examples include hydroxychloroquine and methotrexate.
Biologics
Biologics or biologic response modifiers target various protein molecules involved in the immune response to reduce inflammation and other symptoms of rheumatoid or psoriatic arthritis. They may be used along with DMARDs. Most of these drugs are administered intravenously.
Examples include Enbrel (etanercept), Actemra (tocilizumab), Xeljanz (tofacitinib) and Humira (adalimumab).
Corticosteroids
These drugs reduce inflammation and suppress the immune system. This class of drugs includes prednisone and cortisone. These drugs may be injected into the joint or taken orally.
Surgery
If medication isn’t enough, a doctor may recommend joint replacement surgery. The most common joint replacements are hip replacement and knee replacement. But surgeons can also perform shoulder replacement or elbow replacement.
Surgeons will remove damaged joints and replace them with implants. These surgeries improve mobility and relieve pain. But like any surgery, they may have complications. Implants may be faulty and fail early. When this happens, revision surgery is needed to replace the faulty joint.
- Joint dislocation
- Implant failure
- Blood vessel and nerve injury
- Loosening of the implant
- Blood clots
- Infection
Physical and Occupational Therapy
Physical therapy works to treat arthritis by improving the strength and mobility of joints with special exercises. A physical therapist will tailor the exercises to each patient depending on their needs. Regular therapy can help reduce symptoms of pain and inflammation.
Occupational therapy teaches patients how to change their workplace and home environments to help them reduce motions that can worsen arthritis. They also help people learn how to use assistive devices to help them do daily tasks like dressing, bathing and cleaning the house.

Living with Arthritis
While arthritis can be painful, there are things people can do to feel better and improve their quality of life.
- Follow instructions on how to take medication and make sure you don’t miss doses.
- Try relaxation therapy, gentle stretching and meditation to help reduce pain by learning ways to relax your muscles.
- Ask your therapist about assistive devices such as a shoe insert or cane to ease pain while walking. Other devices can help you close zippers, open jars or hold pencils.
- Cold and heat therapies will help reduce joint pain and swelling.
- Braces and splints can support weakened joints and allow them to rest. Your doctor or therapist can help you find a brace or splint that fits correctly and gives you proper support.
Lifestyle Changes
For patients with milder forms of arthritis, lifestyle changes are the first line of treatment. These strategies can also be helpful for more advanced stages of disease.
Healthy Diet
Eating plenty of fruits, vegetables, whole grains and fatty fish like salmon and tuna may help control inflammation. Eating healthy may help control weight and put less strain on the joints.
Avoid eating foods that can trigger inflammation and weight gain. These include saturated fats, added sugar, refined carbohydrates and an additive called monosodium glutamate (MSG) that may trigger chronic inflammation.
If you have arthritis, it’s best to minimize alcohol consumption because alcohol may also trigger inflammation.
Regular Exercise
Exercise helps people maintain a healthy weight, but it also keep joints functioning properly. Physical therapists help patients develop a therapeutic exercise routine that focuses on joints and flexibility.
In addition to therapeutic exercises, people can include recreational exercises such as swimming, water aerobics, biking and walking.
Always talk to your doctor before starting a new routine.
Ways to Relieve Pain
In addition to over-the-counter medications like Tylenol or ibuprofen, and getting more physical activity, the CDC recommends some non-medication strategies for controlling pain, such as attending education workshops.
These workshops — such as the Chronic Disease Self-Management Program (CDSMP) — teach people life skills for coping with arthritis pain.
According to the CDC, people who participated in these workshops had significant improvements in physical health, including less pain and increased ability to do house work and social activities. They also reported mental health benefits such as decreased worry, fear and depression.
Cognitive behavioral therapy is a psychological, goal-directed approach for managing arthritis pain. Patients learn to modify behavioral, physical and emotional triggers of pain and stress.
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.

