Psoriatic Arthritis
Psoriatic arthritis (PsA) is a type of chronic arthritis that affects the joints. It usually affects people with psoriasis, an autoimmune disease that causes red, scaly patches of skin, but can occur in people without it. This inflammatory arthritis can affect any joint in the body, but typically affects the fingers and toes.

Studies estimate about eight million people in the United States have psoriasis, and 10 to 30 percent of these people develop psoriatic arthritis, according to the National Psoriasis Foundation.
The disease causes inflammation, swelling, pain and stiffness in the joints. It’s often mild, according to the National Library of Medicine. But without treatment, severe forms of the disease can cause permanent, disabling joint damage.
The disease typically starts about 10 years after someone begins showing signs of psoriasis. In about 15 to 20 percent of people, arthritis begins before psoriasis. Some people have both at the same time.
While children can develop PsA, it usually manifests in people ages 30 to 50. The disease affects men and women equally.
There is no cure for PsA, but early diagnosis and treatment can prevent permanent joint damage. Treatment focuses on managing symptoms and slowing disease progression.
Symptoms and Signs
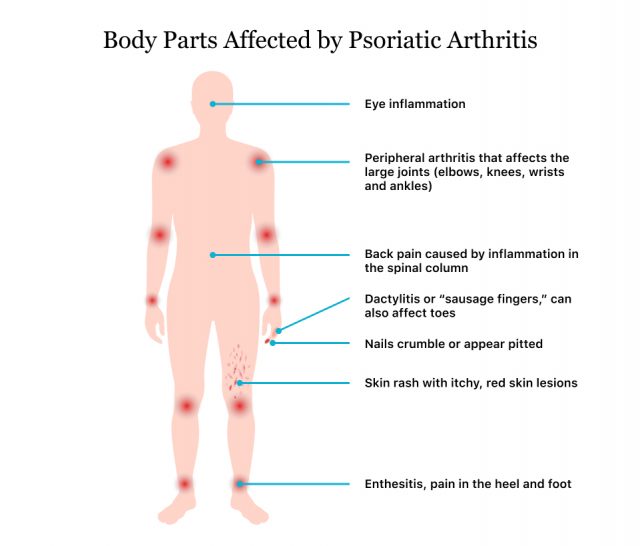
Psoriatic arthritis symptoms may affect the joints on one or both sides of the body. It can cause problems in any joint or where tendons or ligaments connect to bones.
The first signs of PsA are painful, swollen joints that feel warm to the touch. About 35 percent of people have dactylitis, a condition where fingers and toes swell up and look like sausages.
- “Sausage fingers” — swollen fingers and toes that are difficult to bend and look like sausages
- Changes in nails such as nail separation or pitting that mimic fungus infections
- Fatigue
- Morning tiredness and joint stiffness
- Reduced range of motion
- Swelling, pain and tenderness over tendons
- Throbbing, swelling, stiffness, pain and tenderness in one or more joints
- Uveitis, pain and redness of the eye
Types of PsA
There are five subtypes of psoriatic arthritis. Mild psoriatic arthritis that affects four or fewer joints is referred to as oligoarticular, and severe psoriatic arthritis that affects four or more joints is referred to as polyarticular.
Symmetric Polyarthritis-Predominant Arthritis
This type affects five to 10 percent of people with PsA, according to the Cleveland Clinic. The National Psoriasis Foundation, however, estimates it affects about 50 percent of people with PsA. This type affects the same joint on both sides of the body, similar to rheumatoid arthritis. Symptoms usually affect hands, wrists, feet and ankles.
Asymmetric Oligoarthritis or Monoarthritis
This is the most common subtype, and it affects 70 to 80 percent of people with PsA, according to Cleveland Clinic. Hands and feet are most often affected. Symptoms can affect one to three joints.
Distal Interphalangeal Predominant
This type of PsA affects 10 percent of cases. It affects distal joints, the joints closest to the nails. Fingernails and toenails may lift up from the nail bed and appear discolored and pitted.
Spondylitis
Spondylitis is a type of PsA that affects the spine. It causes stiffness in the back and difficulty moving, especially in the morning. Symptoms affect the lower back and neck, but other joints may also be affected. It affects about five to 20 percent of people.
Psoriatic Arthritis Mutilans
This type of PsA is a rare, painful type that may cause deformation, especially in the hands. It typically affects the feet and hands but may also affect the lower back and neck.
Causes and Risk Factors
Researchers aren’t sure what causes psoriatic arthritis, but they know it occurs when the immune system attacks healthy tissues and cells. It causes joint inflammation as well as abnormal overproduction of skin cells.
Several risk factors make someone more likely to get the disease.
- Psoriasis
- Having psoriasis is the biggest risk factor for developing PsA. About one in four people with psoriasis has PsA, according to the Journal of the American Academy of Dermatology.
- Race
- Whites are more likely to get PsA than Asians or African Americans.
- Family History
- People who have family members with PsA are more likely to get it.
- Age
- People ages 30 to 50 are most likely to develop PsA.
Common Triggers
Psoriatic arthritis flare-ups can be triggered by environmental factors. These triggers vary from person to person.
Skin Injuries
Injuries to the skin such as infections, wounds, sunburns or surgery can trigger PsA.
Stress
Stress is one of the biggest factors implicated in PsA flare-ups. Stress causes an increase in inflammation, which can cause the first flare-up as well as subsequent flare-ups. Lack of sleep can also contribute to the body’s stress level and increase the risk of flare-ups.
Medications
Side effects of taking or stopping medications may cause flare-ups. Some medications that could trigger PsA are lithium, hydroxychloroquine and propranolol. People who use prednisone may suffer a flare when stopping the medication.
Alcohol
Heavy alcohol consumption may make preexisting psoriasis worse, according to a 2011 study in the International Journal of dermatology.
Diagnosis
There is no specific test for psoriatic arthritis. Medical providers diagnose the disease based on family history, a physical exam, blood or fluid samples and X-rays to differentiate it from other diseases such as gout, rheumatoid arthritis and reactive arthritis. Dermatologists may screen for the condition, but it is usually diagnosed by a rheumatologist.
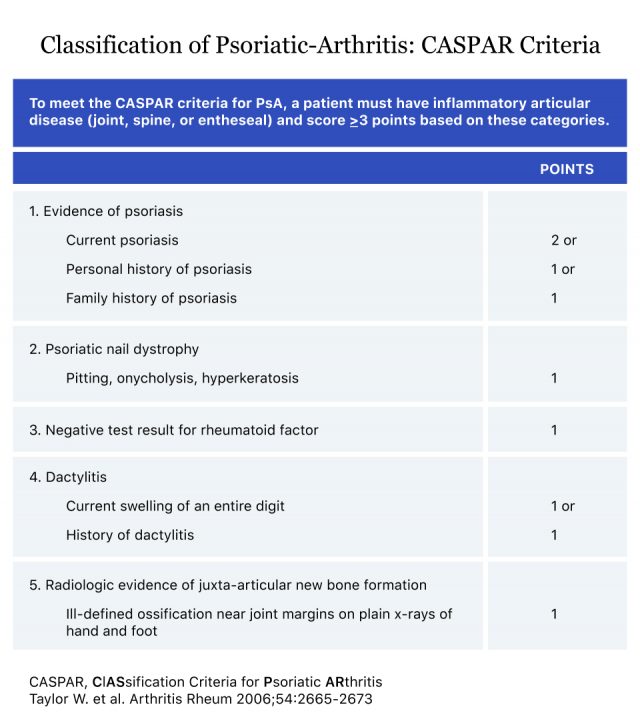
There is no official diagnostic criteria for PsA, but many doctors use a scoring system called the Classification Criteria for Psoriatic Arthritis (CASPAR) to help them diagnose the disease. A PsA diagnosis requires a person to have an inflammatory disease and score three or more on the CASPAR.
Prognosis and Treatment
Psoriatic arthritis is a chronic condition that affects quality of life and causes disability in some cases. Some evidence suggests that people with PsA have a slightly shorter life expectancy. But, generally, people can manage their symptoms with medication and lifestyle changes. It has a slightly better prognosis than rheumatoid arthritis because it affects fewer joints.
Since there is no cure for PsA, treatment focuses on managing symptoms and stopping joint degeneration. Treatment options include medications, joint injections and surgery.
Medication
Medication is often the first line of treatment.
Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
Over-the-counter NSAIDs such as Aleve (naproxen sodium) and Advil (ibuprofen) can help reduce inflammation and pain. In more severe cases, a doctor may prescribe a stronger NSAID.
Immunosuppressants
Immunosuppressants suppress the immune system to control inflammation and other symptoms of PsA. Examples include cyclosporine and azathioprine. Because they suppress the immune system, they may also increase the risk of infection.
Disease-modifying Antirheumatic Drugs (DMARDs)
DMARDs slow the progression of PsA and protect joints from more severe damage. Examples include methotrexate, sulfasalazine and leflunomide.
Biologics
Biologics target parts of the immune system that lead to joint damage and trigger inflammation. Like DMARDs, they may increase the risk of infection.
Coping with Psoriatic Arthritis
Living with psoriatic arthritis and coping with its symptoms can be difficult. But people can make a few changes to improve their quality of life.
Learn How to Protect Your Joints
If you have pain in your joints, try to learn new ways to do daily activities that put less stress on the joints. For example, open doors with the whole body instead of just the hands or fingers. Lift heavy objects with both hands instead of one. Use jar openers to help you in the kitchen.
Occupational therapists can help you learn how to move in new ways to protect yourself.
Maintain a Healthy Weight
Losing weight puts less strain on your joints and may help your medications work better. Medications, including those for psoriatic arthritis, may not work as well in overweight people.
Exercising and eating plenty of vegetables, fruits and proteins will help you maintain a healthy weight and keep joints flexible and muscles strong. Try exercises such as swimming, walking and biking that are low impact.
Stop Smoking and Limit Alcohol
Smoking and heavy alcohol use increase the risk of psoriasis and can make the disease worse.
Get Rest and Manage Stress
Get plenty of rest and sleep when you feel tired. In addition, flare-ups may increase fatigue. Make sure to get more rest during a flare-up.
Stress is one of the biggest PsA triggers. Taking the steps to improve mental health and decrease stress will help manage flares. Try meditation or deep breathing techniques a few times a day when you feel overwhelmed.
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.

