Rheumatoid Arthritis
Rheumatoid arthritis (RA) is a long-term autoimmune disorder that causes the immune system to attack healthy tissues in joints such as the hands, wrists, feet, spine, knees and jaw. RA is a progressive disease that usually affects joints on both sides of the body.

About 1.5 million Americans have RA, according to the Arthritis Foundation. Arthritis most commonly affects older people, but RA can start at any age. It affects both women and men, but it’s three times more likely to develop in women.
Unlike the most common type of arthritis, osteoarthritis, RA symptoms include fatigue, fever and a loss of appetite in addition to painful, stiff joints. If people experience pain in a joint on one side of the body, it is likely to also affect the same joint on the other side of the body.
There is no cure for RA, and it’s a progressive disease — meaning it gets worse over time. Severe forms of the disease can be disabling and disfigure joints. People cannot die from rheumatoid arthritis, but it can cause complications that may be life-threatening.
Treatments can help people with the disease lead productive lives, and early diagnosis helps control joint damage before it becomes severe.
Symptoms and Early Signs
Typically, the first sign of rheumatoid arthritis is stiffness, followed by pain and tenderness in the joints. These symptoms can worsen slowly over weeks or months. Most often, symptoms start in smaller joints such as fingers and toes, and then move to other joints.
The number of joints affected varies, but RA most often attacks five or more joints. It may start as swelling that comes and goes, lasting for a few days or weeks at a time, but it gradually gets worse.
Symptoms may also worsen and occur in intense attacks called “flares” when triggered by stress, suddenly stopping medications or too much activity, according to National Institute of Arthritis and Musculoskeletal and Skin Diseases.
- Painful joints when moving and at rest
- Swelling, tenderness and warmth in the joint
- Loss of appetite
- Stiffness in joints that lasts longer than 30 minutes
- Low energy or fatigue
- Low-grade fever
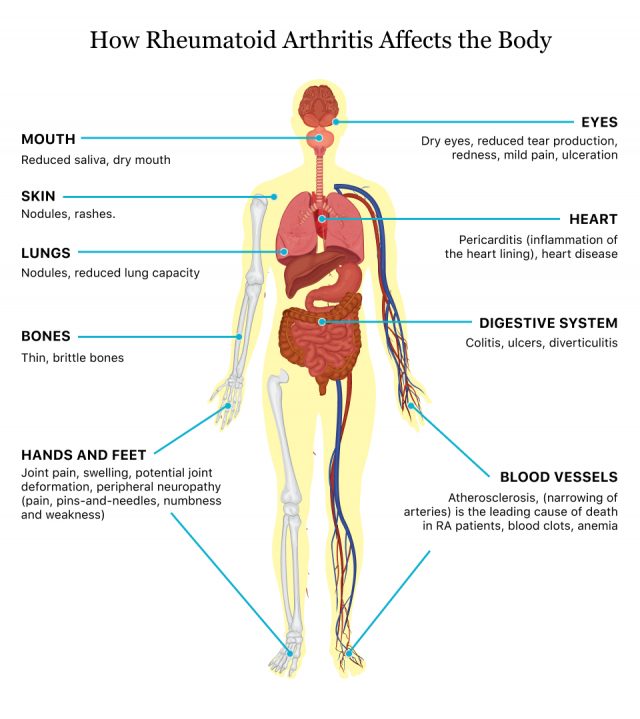
Because RA is an autoimmune disease, it can affect the entire body and attack the eyes, heart, glands, nails and nerves.
Causes and Risk Factors
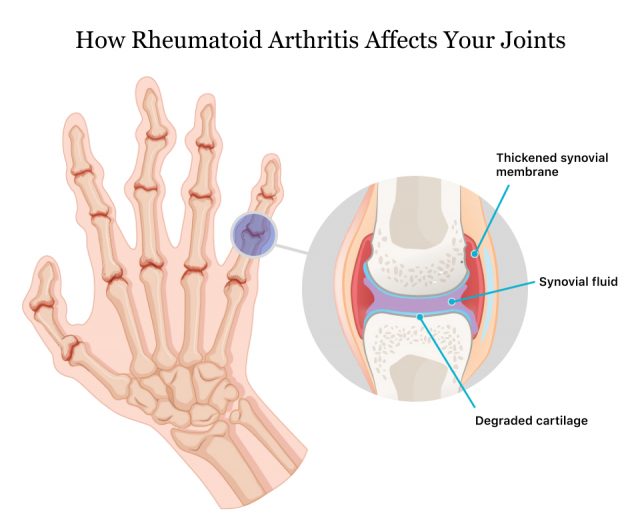
RA is caused when the immune system attacks healthy joint tissues. Researchers don’t know what causes the immune system to attack the synovium, the lining of the joints. But this process involves inflammatory proteins, including tumor necrosis factor-alpha, that can destroy bone and cartilage, stretching and weakening tendons and ligaments.
This leads to pain and loss of joint shape and alignment.
Risk Factors
While researchers don’t know the exact cause, several risk factors can make someone more likely to get RA. Women are more likely to get RA, but according to the Centers for Disease Control and Prevention, women who breastfed their infants have a decreased risk.
- Age
- While RA can affect people of all ages, the risk of developing it increases with age, especially for adults in their 60s.
- Female Sex
- Women are 2-3 times more likely to have RA than men.
- Smoking
- People who smoke are more likely to develop RA, and smoking makes symptoms worse. Children exposed to secondhand smoke have double the risk of developing RA.
- Never Given Birth
- The risk of RA may be greater in women who have never given birth.
- Environmental exposures
- Exposure to toxic substances such as chemicals, asbestos or silica may increase the risk of developing rheumatoid arthritis.
- Obesity
- Being overweight increases the risk of RA, especially in women 55 or younger.
Is It Hereditary?
Research suggests that people born with specific genes called HLA (human leukocyte antigen) class II genotypes are more likely to develop RA. These genes can also make symptoms worse. In people who are obese or who smoke, the risk is highest.
People with relatives who have RA are also at increased risk of developing the disease.
Complications
People with rheumatoid arthritis are at risk of developing other health problems. In addition to physical issues, people with RA can also have difficulty keeping or finding employment because of physical limitations such as pain and fatigue.
- More body fat
- Carpal tunnel syndrome
- Dry eyes and mouth, a disorder called Sjogren's syndrome
- Heart problems
- Infections
- Lung problems such as scarring and shortness of breath
- Lymphoma, a type of blood cancer
- Osteoporosis, a condition that makes bones weak and more prone to breaking
Types
There are three main types of RA. While symptom severity in each type may be different, the treatments are the same.
Seropositive RA
About 80 percent of people with RA have this type of disease, according to the Illinois Bone & Joint Institute. This means blood tests showed a protein called rheumatoid factor (RF) and antibodies called anti-citrullinated protein antibodies (ACPAs). This type of RA can have more severe symptoms than seronegative RA.
Seronegative RA
People with this type of RA don’t test positive for antibodies or proteins, but they still have RA symptoms. They are also less likely to have complications such as lung issues, heart problems and inflamed blood vessels.
Juvenile Idiopathic Arthritis (JIA)
Juvenile idiopathic arthritis affects children ages 17 years old and younger and may sometimes be called juvenile rheumatoid arthritis. It has many of the same symptoms as adult RA but can also cause difficulty gaining weight and growing. Unlike adult RA which is a lifelong condition, children can outgrow JIA.
How Is RA Diagnosed?
Doctors that specialize in diagnosing RA and other types of arthritis are called rheumatologists. If your primary care provider suspects you might have RA or another type of arthritis, he or she may refer you to a rheumatologist for testing.
A rheumatologist will diagnose RA based on several tests. These include blood tests, imaging tests such as X-rays and MRIs and a physical examination.
Blood tests search for a protein called rheumatoid factor (RF) and antibodies called anticitrullinated protein antibodies (anti-CCP). Other tests such as the erythrocyte sedimentation rate (ESR) test and C-reactive protein test can find high levels of inflammation present in people with RA.
These tests also help doctors distinguish RA from other types of arthritis such as gout, osteoarthritis, lupus and psoriatic arthritis.
Four Stages of RA
RA has four stages that progress in severity. The stage of disease can influence treatment.
- Stage 1
- Early stage RA with some swelling and stiffness in joints.
- Stage 2
- Moderate stage RA with cartilage damage. Difficulty moving joints occurs more often.
- Stage 3
- Severe disease that destroys bone and cartilage. Increased pain, swelling, decrease in mobility and loss of muscle strength. Joints may begin to deform.
- Stage 4
- End stage RA where joints stop functioning. Symptoms include severe pain, swelling, stiffness and loss of mobility.
Rheumatoid Arthritis (RA) vs. Osteoarthritis (OA)
People with RA and OA have pain in the joints and difficulty moving around, but there are a few differences in severity of symptoms and how they manifest.
| Characteristic | RA | OA |
|---|---|---|
| Age when symptoms begin | Any time in life | Usually affects older people |
| How long morning joint stiffness lasts | Lasts for more than an hour | Lasts less than an hour |
| Joint symptoms | Pain, swelling and stiffness | Pain, tenderness but little to no swelling |
| How joints are affected | Affects small and large joints on both side of the body in a symmetrical pattern, such as both elbows, wrists, hands or balls of the feet | Symptoms begin on one side of the body and may spread gradually to other side. Symptoms begin gradually and usually affects one set of joints such as joints closest to fingernails or large weight-bearing joints such as hips, knees or spine |
| Whole body symptoms | General feelings of being ill and tired | Doesn’t affect the whole body |
| How fast do symptoms develop | Quickly over weeks or months | Slowly over years |
Treatment Options
Treatment options for RA include medication, occupational therapy and surgery. In addition, lifestyle changes and assistive devices are things people with RA can do to manage symptoms at home.
Doctors will prescribe treatments depending on the stage of disease, severity of symptoms and degree of inflammation.
Medications
Several types of medications treat RA, and a doctor considers how long a patient has had the disease and the severity of symptoms when choosing a medication. Sometimes, people may have more than one prescription.
Nonsteroidal anti-inflammatory drugs (NSAIDs)
Over-the-counter NSAIDs such as ibuprofen (Advil, Motrin IB) and naproxen sodium (Aleve) can relieve pain and inflammation. Stronger NSAIDs are available by prescription.
Corticosteroids
These medications, such as prednisone, reduce pain and inflammation. They can also slow joint damage. These medications are usually prescribed for acute symptoms and patients gradually stop them.
Disease-modifying antirheumatic drugs (DMARDs)
DMARDs can slow the progression of RA and save tissues and joints from permanent damage. Common DMARDs include methotrexate and hydroxychloroquine, also known as Plaquenil.
Biologics
These drugs, also known as biologic response modifiers, are a newer class of DMARD. They target parts of the immune system to control joint and tissue damage. Drugs in this class include Humira (adalimumab), Enbrel (etanercept), Remicade (infliximab), Actemra (tocilizumab) and Xeljanz (tofacitinib).
Occupational Therapy
Occupational therapists can help people with RA learn to better manage their symptoms. Patients can learn how to do daily chores with less pain, how to protect their joints and how to use assistive devices to make daily tasks easier. Evidence from studies shows that occupational therapy helps people with RA do daily chores without pain and better protect their joints, according to a Cochrane review.
Surgery
In cases of severe RA disease, surgery may be able to help regain some mobility and decrease pain.
Arthroscopy
In this procedure, surgeons remove damaged or inflamed tissue without replacing or reconstructing a joint. It can restore joint function and relieve pain.
Nerve Release
This type of surgery is also called nerve decompression surgery. It helps relieve pain caused by impinged nerves. This restores strength to the affected joints affected by RA, including elbows, feet, toes and wrists.
Synovectomy
A synovectomy is surgery to remove the diseased synovial lining in a joint. It reduces swelling, alleviates pain, and can help prevent or slow down damage to the joint.
Hand and Wrist Surgery
Hand and wrist surgery can repair damaged tendons and ligaments in the hands. It helps restore movement to the joints in the hands, wrists and fingers.
Arthroplasty
In arthroplasty, the affected joint is replaced or reconstructed. This surgery can restore joint function, fix a deformity, relieve pain and stiffness, and improve mobility.
Home Remedies for Managing RA
In addition to medication and surgery, patients may want to ask their doctor about simple therapies they can do at home, such as exercise and diet.
Exercise
Low impact exercises can strengthen muscles and improve flexibility. These include walking, water aerobics, swimming and yoga.
According to a 2012 review published in Open Access Journal of Sports Medicine by Shirley Telles and Nilkamal Singh, yoga has shown some promise in reducing pain, improving function and providing mental health benefits.
A small 2019 study by researcher Surabhi Gautam and colleagues published in Restorative Neurology and Neuroscience found that yoga eased physical symptoms and improved mental health.
Diet
Evidence suggests that eating a healthy diet with anti-inflammatory foods can ease RA symptoms. There isn’t a specific regimen to follow, but a 2018 review recommended the Mediterranean diet and fish oil for people with RA, Today reported.
In general, keeping a healthy weight and getting the proper nutrition helps manage inflammation that can worsen RA.
- Fatty fish like salmon, sardines and tuna
- Fruits and vegetables
- Whole grains
- Beans and peas
- Nuts
- Olive oil
Getting Enough Sleep
People with RA often suffer from fatigue and pain that can get worse during flare-ups. Make sure to get plenty of rest.
Hot and Cold Therapy
Heating pads or warm showers and cold packs can help ease inflammation, pain and stiffness.
Assistive Devices
Assistive devices such as canes, splints and braces can ease strain on joints and keep them in proper alignment. Household aids such as handrails or grab bars can help people stay safe and prevent injury.
Occupational therapists can help people learn how to use assistive devices.
Improving Quality of Life
RA symptoms can affect all aspects of a person’s life, including work, social and leisure activities. The CDC has recommendations for improving quality of life for people with RA.
Start an Exercise Plan and Stay Active
Aim to stay active for 30 minutes a day, five days a week. These 30-minute sessions can be done all at once or broken up into 10-minute sessions throughout the day.
Walking, swimming, yoga or bicycling can be effective exercises to improve cardiovascular health, flexibility and muscle strength in people with RA. Always check with your doctor before starting an exercise routine.
Participate in Group Activities
If exercising alone seems daunting, join a group fitness class or activity session at a local community center or other facility. These classes can teach people how to exercise effectively and safely. Plus, meeting with others can help improve mood.
Physical therapists may also be able to teach a person with RA how to properly exercise to help reduce pain and increase mobility.
Enroll in a Self-Management Education Class
People with RA who take a self-management class can learn more about arthritis, learn tips for living with the disease and learn how to control symptoms. Examples of CDC-recommended programs include Arthritis Self-Management Program (ASMP) and Chronic Disease Self-Management Program (CDSMP).
Learn more about CDC-recognized programs proven to teach people with RA and arthritis how to manage their conditions.
Quit Smoking
Smoking increases the severity of RA symptoms and can cause other medical problems. Ask your doctor for help in quitting or visit the CDC’s How to Quit Smoking page.
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.

