Deep Vein Thrombosis
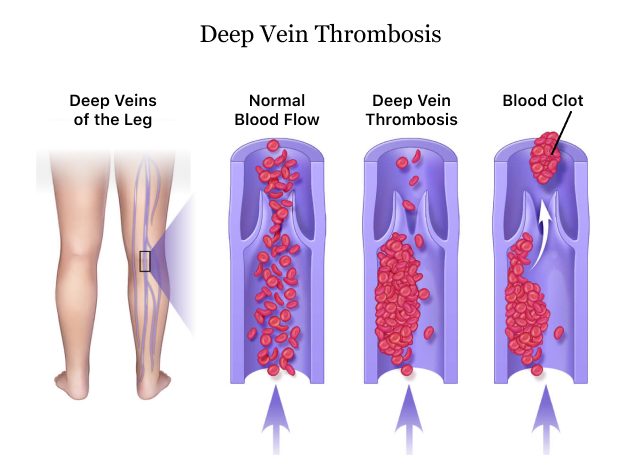
A deep vein thrombosis, or DVT, is a blood clot that forms in the deep veins of the body, usually in the thigh, calf or pelvis. Symptoms include swelling, pain, tenderness or red skin. Other names for DVT include thromboembolism and venous thromboembolism.
Though the precise number of Americans with DVT is not known, about 1 in 1,000 people develop a DVT with symptoms each year, according to information provided by the Institute for Quality and Efficiency in Health Care (IQWiG), published by the U.S. National Library of Medicine.
While there are a few risk factors for DVT, having surgery that involves your hips or legs or experiencing an injury to your lower body are two of the most common. This is why most people receive anticoagulants such as warfarin or Xarelto to prevent blood clots after hip replacement or knee replacement surgery.
DVTs usually go unnoticed and dissolve on their own. But blood clots that remain in the vein can cause damage to the blood vessel.
Symptoms and Complications
The symptoms of DVT affect the leg with the blood clot, though some people might not have any symptoms. For those people, complications of DVT might be the first symptoms they experience.
- Bulging veins
- Discolored, red or tight skin
- Edema or swelling
- Tenderness and pain
- Thickening of veins called "cords"
- Warmth in the affected area
Complications of DVT
These types of blood clots don’t cause heart attacks or strokes. But DVT can cause long-term health problems including pulmonary embolism, post-thrombotic syndrome and postphlebitic syndrome. About 33 percent of people with DVT will have a recurrence within 10 years.
Pulmonary Embolism (PE)
Up to 100,000 people die of DVT or one of its more deadly but rare complications, pulmonary embolism (PE), according to the Centers for Disease Control and Prevention.
A PE occurs when a DVT travels to the lungs and blocks blood flow. The risk is greater if the DVT is in the pelvis or upper part of the leg. A pulmonary embolism requires emergency treatment.
- Feeling lightheaded or dizzy
- Losing consciousness
- Low blood pressure
- Pain in the chest, especially when coughing or breathing in
- Rapid heartbeat
- Shortness of breath that can come on suddenly
- Coughing up blood (rare)
Post-Thrombotic Syndrome (PTS)
A lot of people who suffer DVTs recover. But up to half may develop a complication called post-thrombotic syndrome (PTS), a condition that causes swelling, chronic pain and discomfort, according to Boston Scientific.
These symptoms are caused by damage to the valves in the veins. This causes problems with normal blood flow.
Postphlebitic Syndrome
About 20 to 50 percent of people who have DVT may suffer from postphlebitic syndrome. This usually occurs within 1 to 2 years after severe DVT, according to Merck Manual.
- Aching
- Cramps
- Feeling of “pins and needles”
- Fullness
- Heaviness
- Pain
- Tiredness
Symptoms usually get worse with walking or standing but may feel better with elevating the leg or sitting. These symptoms worsen with standing or walking and are relieved by rest and elevating the leg. Some people may develop a skin rash on the lower legs or ankles.
How Are DVTs Diagnosed?
Health care providers diagnose people with DVT based on symptoms and physical examination. If the provider suspects a DVT, they will order tests. Three of the most common tests are duplex ultrasound, magnetic resonance imaging and venography.
Duplex Ultrasound
A duplex ultrasound combines traditional ultrasound technology — using sound waves that echo off the body — with Doppler technology to generate a color image of blood flow. It’s noninvasive, painless and doesn’t require radiation.
Magnetic Resonance Imaging (MRI)
MRIs produce detailed images of structures inside the body, including veins, using magnetic fields. An MRI can take images of both legs at the same time. Like an ultrasound, the test is noninvasive and painless. However, some patients with implanted devices might not be able to do an MRI.
Venography
Venography is an invasive procedure that requires an injection of contrast dye into a vein in the foot. After the dye mixes with blood, the health care provider uses an x-ray to observe the blood flow. Because it’s invasive and requires radiation, venography is rarely used.
Causes and Risk Factors
There are several causes and risk factors for developing a DVT, which occurs when blood cells stick together to form a clot. Anything that affects blood circulation can form a clot, including genetics, lack of movement, injury, illness and lifestyle factors.
Some medications may also increase your risk for blood clots. For example, the U.S. Food and Drug Administration warned that women taking birth control pills containing drospirenone, such as Yaz, may have an increased risk of blood clots.
- Being in bed after an injury or fracture without encouraging blood circulation
- Being in bed after surgery
- Diseases that cause the blood to clot too much
- Extended periods of bedrest without much movement
- Major operations, particularly surgeries of the hip, leg or abdomen
- Serious injuries to blood vessels
- Age, people over 60 have an increased risk
- Certain inflammatory diseases
- Congestive heart failure (CHF)
- Frequent travel with long stretches of sitting
- Genetics and family history
- High levels of cholesterol
- History of DVT
- Hormonal contraception (Yaz, Nuvaring)
- Hormone replacement therapy (HRT), hormone treatment for menopause
- Pregnancy
- Severe obesity or being overweight
- Smoking
- Some cancers
- Varicose veins
Deep Vein Thrombosis Treatment
Some people with DVT don’t require treatment. In these cases, a health care provider will monitor the clot to see if it gets any worse or goes away on its own.
Treatment for DVT focuses on stopping the growth of a blood clot, preventing the clot from traveling to the lungs and reducing the chance of a reoccurring clot.
Medication
Doctors usually recommend medications as the first line of treatment. Anticoagulants, or blood thinners, help dissolve existing clots and prevent new clots from forming. All blood thinners have a risk of causing internal bleeding.
Older medications like heparin and warfarin require blood tests to get the correct individual dose. Doctors will start with heparin and then follow up with warfarin. These medications require routine tests to monitor levels of anticoagulation and dosing may be adjusted depending on test results. Warfarin also requires dietary changes to make sure it stays effective.
Newer blood thinners called Factor Xa inhibitors such as Xarelto (rivaroxaban) and Eliquis (apixaban) don’t require blood tests, because they are a one-size-fits-all medication. They don’t require dietary changes to be effective.
In people who are at extremely high risk for PE or extremely large clots, a health care provider may recommend “clot buster” drugs called thrombolytics. These drugs include streptokinase and alteplase. Doctors deliver the drug directly into the clot through a catheter.
Compression Devices
Most people do well with anticoagulant therapy and compression or support stockings to improve blood flow and reduce swelling. The compression prevents blood from pooling in the veins and helps circulation.
After surgery, some people may use an external pneumatic compression device to prevent clots. This device resembles a boot. It applies pulses of pressure to the calf and simulates muscles pressure from walking to prevent clots and stimulate blood flow.
IVC Filters
Inferior vena cava or vena cava filters are small metal cage-like devices with spidery legs. Surgeons implant these into a vein to act as a trap for blood clots and prevent them from lodging in the heart and lungs.
Rarely, these devices may perforate the vein. Some may break, and the small fragments may lodge in the heart and other organs. Some devices have greater failure rates than others and patients should be aware of the brand their surgeon recommends.
Raise and lower toes while keeping heels on the floor
Tighten and release leg muscles
How to Prevent DVT
Because DVT can lead to several serious conditions and might not always have symptoms, the best thing for people to do is prevent them. People can prevent DVT by maintaining good cardiovascular health, a healthy body weight and avoiding inactivity.
- Avoid sitting for too long without moving. Periodically get up at work or at home. Taking short walks or performing activities that contract leg muscles keep the blood flowing back to the heart.
- Being overweight or obese increases DVT risk. Make lifestyle changes to lose weight or maintain a healthy body weight. Ask your doctor for a nutritionist or dietician who can help couch you.
- Dehydration may increase your risk for blood clots. Make sure you drink plenty of water, especially when sitting for prolonged periods.
- If you are bedridden and can’t walk, prevent your blood from pooling and clotting by contracting leg muscles.
- If you are bedridden in a hospital, make sure doctors and nurses take steps to prevent clots such as taking medication, wearing compression stockings or using an external pneumatic compression device to massage your calves and keep blood circulating.
- If you are taking a long car ride, make sure you take breaks and get out to stretch and walk for a few minutes. If travelling by plane, try to stand up and walk in the aisles or pump your leg muscles.
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.

