Chronic Pain
Chronic pain, which affects nearly a fifth of U.S. adults, significantly impairs quality of life. It's linked to various medical conditions, injuries and medical devices. An effective chronic pain management strategy involves medications, lifestyle changes and psychological support.

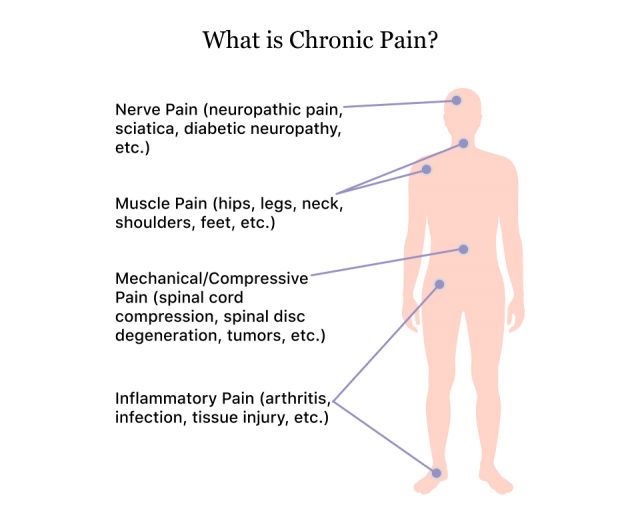
What Is Chronic Pain?
Chronic pain persists for several weeks or months. It may also accompany an underlying health condition.
“Chronic pain is a prolonged form of pain that persists for 12 weeks or longer, often continuing even after the typical recovery period for an injury or illness,” Dr. Taher Saifullah, founder of the Spine and Pain Institute in Los Angeles, told Drugwatch. “This type of pain can occur without a specific cause and may be constant or come in waves, varying in intensity.”
Depending on the cause, chronic pain may be constant or intermittent. According to the Centers for Disease Control and Prevention, in 2021, approximately 20.9% of U.S. adults experienced chronic pain and an additional 6.9% experienced high-impact chronic pain.
“Chronic pain can significantly impair quality of life, leading to issues like disrupted sleep, depression and reduced physical functionality,” Dr. Saifulla said.
Chronic pain can impact physical and mental health, which may lead to reduced activity, fatigue, depression and substance abuse. It is important to manage these symptoms.
A 2024 study by researchers at the University of Texas Southwestern Medical Center found that aging African Americans with supportive family relationships are less likely to develop chronic pain, while those with strained relationships are more likely to suffer from it.

Causes of Chronic Pain
Health conditions like arthritis, cancer and migraines, as well as medical treatments like chemotherapy and surgery, can cause Chronic Pain.
People with acute injuries may develop chronic pain due to improper healing, nerve damage or unknown causes.
Devices Known To Cause Chronic Pain
Medical devices can cause chronic pain due to device failure, improper healing after insertion or site trauma. This is common with joint replacements and mesh implants.
Joint replacements are common procedures, with the American College of Rheumatology reporting Americans undergoing approximately 790,000 knee replacements and 544,000 hip replacements each year. Despite their prevalence, joint replacement is a common cause of chronic pain.
Some patients suffer from persistent postoperative pain, while others may experience nerve damage during the procedure. Many individuals affected by defective hip replacements received compensation through legal settlements. As of February 2025, there were 2,211 active hip replacement lawsuits seeking to hold manufacturers accountable for faulty products.
Hernia mesh and transvaginal mesh are implant devices with a history of complications, including chronic pain. According to a study published in the Journal of Pain Research, up to 16% of patients who undergo inguinal hernia repair experience chronic postoperative pain.
Manufacturers have recalled several types of hernia mesh products because of device failures. As of February 2025, there were multiple multidistrict litigations with a total of 26,278 hernia mesh lawsuits seeking compensation on behalf of affected patients.
Inferior vena cava (IVC) filters are a common cause of postoperative pain and complications. There are active IVC filter lawsuits on behalf of patients who experienced pain and other complications after receiving these devices.
Diseases and Conditions That Cause Chronic Pain
Chronic pain can be caused by medical conditions. Often, it can be the dominant symptom for conditions such as arthritis, cancer, fibromyalgia and migraines.
There are two main kinds of physical pain: nociceptive and neuropathic.
Physical injuries can lead to nociceptive pain, which is when pain receptors outside of the main nervous system activate. Normally, these receptors deactivate once an injury heals. If they instead remain active, individuals may experience pain long after injury recovery.
Neuropathic pain is associated with damage to the neurological system. Factors such as injuries, certain medications and health conditions such as diabetes can cause neuropathic pain. Potential triggers, like wearing socks or laying a bedsheet over your legs, can be subtle. This type of chronic pain can flare up without any apparent cause.
Chronic pain can contribute to mental health problems, leading to feelings of frustration, anger and sadness, which can lead to depression and anxiety. These mental health issues can worsen pain symptoms, creating a cycle of worsening conditions.

Symptoms and Diagnosis of Chronic Pain
Chronic pain symptoms vary based on causes, location and other health conditions. Pain from a medical device is typically felt in the affected area, while neuropathic pain may be more widespread.
- Arthritis, or joint pain
- Back pain
- Cancer pain near a tumor
- Headaches, including migraines
- Lasting pain in scar tissue
- Muscle pain all over (such as with fibromyalgia)
- Neck pain
- Neurogenic pain from damage to the nerves or other parts of the nervous system
- Testicular pain (orchialgia)
Chronic pain lasts at least three months and can vary in intensity. It may be accompanied by depression, anxiety and mood changes. Seek a chronic pain diagnosis to manage your symptoms.

Managing Chronic Pain Effectively
Maintaining overall mental and physical health is important for managing chronic pain. Strategies include medications, lifestyle changes, mind-body therapies and behavioral treatments.
“[Over-the-counter] pain relievers are commonly used to manage both acute and chronic pain, but their effectiveness and safety profiles may vary,” Kate Moore, a spokesperson for AICA Orthopedics in Atlanta, told Drugwatch. “Chronic pain management may require prolonged use, leading to a higher risk of side effects and necessitating a more comprehensive treatment approach.”
Pharmacological interventions are common in pain management. Many patients rely on over-the-counter options such as acetaminophen, NSAIDs and topical pain creams.
“OTC pain relievers are usually used for acute pain episodes and give symptom relief,” Dr. Su Hlaing Hnin, a board-certified internal medicine physician with Medical Offices of Manhattan, told Drugwatch. “Most OTC pain relievers are not safe or meant to be used for the long run.”
Doctors frequently prescribe opioids, muscle relaxers, anticonvulsants and corticosteroids for pain. Sedatives and antidepressants can help relieve symptoms such as insomnia and depression.
Lifestyle changes may involve exercise, heat/cold therapy and a balanced diet. Complementary treatments like acupuncture and massage can also address chronic pain symptoms.
Patients with emotional symptoms can benefit from psychological support, such as cognitive behavioral therapy, counseling and fear-avoidance training.
Treatment will vary for each patient and should address the symptoms and underlying causes.
Editor Lindsay Donaldson contributed to this article.
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.

