Acid Reflux and GERD
Acid reflux is a common occurrence, but when it becomes chronic, it may develop into GERD. These conditions share similar symptoms, like heartburn, but GERD is more frequent and severe. Understanding their differences and treatments can help manage discomfort and prevent complications.
What Is Acid Reflux and GERD?
Acid reflux, also called gastroesophageal reflux (GER), happens when stomach acid flows back into the esophagus, the tube connecting the throat to the stomach. Gastroesophageal reflux disease (GERD) is a severe form of acid reflux.
This backward flow can cause heartburn, a burning sensation in the chest or throat, especially after eating large meals or consuming alcohol or caffeine.
Anyone can experience occasional acid reflux.
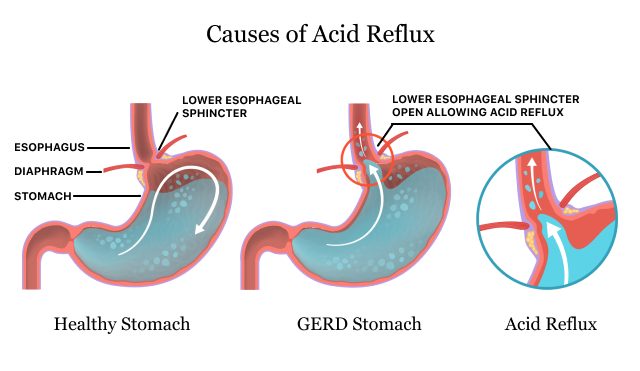
Acid reflux may become GERD when it happens more than twice a week for several weeks. GERD is caused by a mechanical issue where the lower esophageal sphincter doesn’t close properly. This allows acid to escape the stomach frequently.
GERD and Acid Reflux Risk Factors and Lifestyle Changes
Many circumstances, such as eating certain foods or being stressed, can cause stomach acid to back up into the esophagus, triggering acid reflux and GERD. Several factors can play a role in this, but you have the power to make positive changes.
- Aspirin and NSAIDs
- Being overweight or obese
- Drinking alcohol, caffeine or soda
- Eating trigger foods
- Hiatal hernia
- Lying down after eating
- Overeating
- Pregnancy
- Smoking
- Stomach ulcer
- Stress and anxiety
These factors can cause the lower esophageal sphincter (LES) to relax too much or for too long. Common trigger foods include citrus, chocolate, peppermint, and fatty or spicy foods. Carbonated beverages and caffeine could also trigger the acid reflux of GERD.
Those with a hiatal hernia, which is when part of the stomach moves into the chest, are also more prone to acid reflux and GERD. While you might want to reach for over-the-counter pain medication to treat physical discomfort, common pain medicines like aspirin and NSAIDs like ibuprofen could make it worse.
Symptoms of GERD and Acid Reflux
The most common acid reflux and GERD symptom is heartburn, a burning sensation in the chest that can rise into the throat. GERD often involves more frequent and severe symptoms that can disrupt normal activities.
- Asthma or asthma-like symptoms
- Bad taste in the mouth
- Burning sensation in the throat
- Coughing or wheezing, especially at night
- Difficulty swallowing (dysphagia)
- Feeling of a lump in the throat
- Heartburn
- Hoarseness
- Nausea and vomiting
- Regurgitation of stomach contents
- Sore throat
- Toothache
Acid reflux and GERD cause a range of uncomfortable symptoms that can affect daily life and, in some cases, lead to complications.
Prolonged GERD can cause more serious complications like inflammation of the esophagus (esophagitis), ulcers and changes in the esophageal lining that could lead to cancer.
Medications That May Cause or Worsen Acid Reflux
Some drugs, such as antibiotics and NSAIDs, may cause heartburn that feels similar to GERD. Other medications, such as narcotics and blood pressure medications, can relax the lower esophageal sphincter (LSE). This means the sphincter fails to close properly and can cause stomach acid to flow back into the esophagus, causing or worsening GERD.
- Antibiotics
- Used to treat bacterial infections. Antibiotics can cause esophagitis, leading to heartburn and pain.
Examples: Amoxicillin, metronidazole, ciprofloxacin, clindamycin, tetracyclines, rifaximin
- Asthma Medications
- Helps ease asthma symptoms. Asthma drugs may weaken the LES, allowing stomach acid to flow back into the esophagus.
Example: Theophylline
- Benzodiazepines
- Treats anxiety, insomnia and seizures. Benzodiazepines can relax the LES, leading to acid reflux and heartburn.
Examples: Valium (diazepam), restoril (temazepam)
- Bisphosphonates
- Used to slow bone loss in osteoporosis. Bisphosphonates may cause heartburn, esophageal irritation, nausea and stomach ulcers.
Examples: Alendronate, risedronate, ibandronate
- Blood Pressure Medications
- Treat high blood pressure and heart conditions. Blood pressure medications can relax the LES, increasing the risk of acid reflux.
Examples: Calcium channel blockers (e.g., amlodipine), beta blockers
- Iron Supplements
- Used to treat iron deficiency anemia. They may irritate the esophagus, triggering heartburn.
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
- Pain relievers that reduce inflammation. These kinds of pain killers can irritate the esophagus, causing heartburn and potentially damaging the stomach lining.
Examples: Ibuprofen, aspirin, aceclofenac
- Opioids/Narcotics
- Provides pain relief. Opioids and narcotics may relax the LES and slow digestion, leading to reflux symptoms.
Examples: Codeine, hydrocodone-acetaminophen
- Potassium Supplements
- Used for electrolyte balance. Potassium supplements can irritate the esophagus, leading to heartburn.
- Progesterone
- Used in hormone therapies and birth control. This hormone may relax the LES, causing or worsening reflux.
- Tricyclic Antidepressants (TCAs)
- Used to treat depression and anxiety. TCAs may relax the LES, causing delayed stomach emptying and worsening GERD symptoms.
Examples: Amitriptyline, doxepin
Many medications can cause or worsen acid reflux and GERD. They generally do this by irritating the lining of the esophagus. If you experience acid reflux or GERD, you may consider telling your doctor so they can help you get the medicine you need without worsening your condition.
Medications to Treat Acid Reflux and GERD
Acid reflux and GERD can be treated by prescription and nonprescription medications. Options include antacids, histamine (H2) blockers, proton pump inhibitors and prokinetic agents. Prescription medications tend to be stronger than over-the-counter (OTC) options.
Antacids
Antacids neutralize the stomach acid that causes heartburn. They come in liquid and tablet forms and are often available without a prescription. Liquids frequently work faster.
Side effects depend on whether the antacid contains magnesium, calcium or aluminum. Antacids can affect how effective other medications are. If you’re on other meds, you should take them one hour before or four hours after an antacid.
- Alka-Seltzer
- Gaviscon
- Gelusil
- Genexa Antacid
- Mylanta (liquid)
- Pepto-Bismol
- Rolaids
- Tums
H2 Blockers
Histamine-2 (H2) blockers help reduce the amount of stomach acid your body makes. They can help with acid reflux, stomach ulcers, GERD and other stomach problems.
Stomach acid is produced when your body releases H2 after you eat. Normally, H2 binds to H2 receptors in your stomach’s lining. H2 blockers bind to the H2 receptors, and the H2 can’t attach and trigger stomach acid production.
Depending on the brand and dosage, H2 blockers can be OTC or prescription (Rx) medications.
- Axid (nizatidine): Available by prescription only.
- Pepcid (famotidine): Available OTC and by prescription.
- Tagamet (cimetidine): Available OTC and by prescription.
- Zantac 360 (famotidine): Reformulated, available OTC.
H2 Blocker Side Effects
Modern H2 blockers are usually safe but can have some side effects. These include stomach pain, muscle aches, constipation, diarrhea, dry mouth, fatigue and headaches. Older adults with reduced kidney or liver function may experience confusion or slurred speech. Also, some H2 blockers can reduce the effectiveness of other medications, such as SSRI depression medications or the blood thinner warfarin.
Ranitidine was originally the active ingredient in Zantac. Introduced in 1983, it was the first FDA-approved H2 blocker. However, in April 2020, the FDA requested manufacturers to remove it from the market. The agency had found that N-Nitrosodimethylamine (NDMA) levels, which can cause cancer, could increase to unsafe levels over time or in high temperatures. This meant Zantac could accumulate high NDMA levels in storage.
Prokinetics
Prokinetic agents, such as Reglan (metoclopramide), aid in gut motility. This can treat acid reflux and GERD by strengthening your lower esophageal sphincter and moving food along. You still absorb nutrients.
Common side effects can include blurry vision, headaches, fatigue, lethargy and gastrointestinal issues.
Some prokinetics can cause neurological and heart issues, so many of these medications are no longer available. Doctors may prescribe them if other options, like PPIs, aren’t working.
Though still available, Reglan comes with risks. Reglan side effects include drowsiness, fatigue, confusion and restlessness. However, serious side effects, including movement disorders like tardive dyskinesia (TD), have led to numerous Reglan lawsuits.
TD is a potentially irreversible condition involving involuntary muscle movements. The FDA issued a boxed warning due to the risk of TD with long-term use.
Proton Pump Inhibitors (PPIs)
Proton pump inhibitors (PPIs) block the “proton pump” enzyme, which makes stomach acid. Using a PPI can significantly reduce stomach acid without hindering digestion.
- AcipHex (rabeprazole sodium): Available by prescription only.
- Nexium (esomeprazole): Available OTC and by prescription.
- Prevacid 24 HR (lansoprazole): Available OTC and by prescription.
- Prilosec (omeprazole): Available OTC and by prescription.
- Protonix (pantoprazole sodium): Available by prescription only.
PPIs should be used for chronic stomach acid issues, not for occasional heartburn. They are potent but take several days to work, making antacids or H2 blockers better for short-term relief. If used over the long term, you may experience side effects.
- C. difficile
- PPI use correlates with a higher risk of Clostridium difficile infection, which can cause severe diarrhea and other gastrointestinal issues.
- Fracture
- Long-term PPI use may reduce calcium absorption, potentially leading to osteoporosis and increased fracture risk, especially in the hips.
- Iron and B12 deficiency
- Lower stomach acid from PPIs can impair the absorption of iron and vitamin B12, potentially leading to deficiencies over time.
- Pneumonia
- Reduced stomach acid can let bacteria thrive, allowing bacteria to travel up the esophagus and into the lungs.
Common PPI side effects include headache, rash, lightheadedness, nausea, bloating and other stomach issues. Prolonged use can cause infections, cognitive decline and other dangerous issues.
Surgical Treatments for GERD
Surgery aims to strengthen the lower esophageal sphincter to prevent acid reflux. Common procedures include laparoscopic fundoplication, transoral incisionless fundoplication and the LINX Reflux Management System.
- Laparoscopic Fundoplication
- This is the most common surgery for acid reflux and GERD. The surgeon wraps part of the upper stomach (fundus) around the bottom of the esophagus to form a valve between the two organs. This strengthens the LES. This wrap can be complete (Nissen fundoplication) or partial (Toupet fundoplication). Patients are often able to stop taking medications after recovery. Laparoscopic fundoplication can include hiatal hernia repair.
- LINX Reflux Management System
- This involves placing a ring of magnetic beads around where the esophagus and stomach meet. Magnetic attraction keeps the sphincter closed while allowing food to pass through. It is a less invasive option with a quick recovery time. But, it’s not suitable for patients with hiatal hernias larger than three inches.
- Transoral Incisionless Fundoplication (TIF)
- Surgeons perform TIF using an endoscope through the mouth. The procedure tightens the lower esophageal sphincter by creating sutures and folding tissues. Patients often recover quickly.
You may need surgery for GERD if your symptoms aren’t relieved by medications and lifestyle changes. Your doctor may also recommend surgery when a hiatal hernia causes GERD.
When to See a Doctor
You should see a doctor as soon as you suspect you have GERD or if acid reflux is bothering you in general. Seek help if you have frequent or unbearable heartburn not helped by OTC meds or lifestyle changes. Needing medication two or more times per week is a good sign that this may be more than simple acid reflux.
If you experience persistent vomiting, trouble swallowing, hoarseness, loss of appetite or unexplained weight loss, it’s time to get checked out.
Seek immediate help at an emergency room if you have chest pain, shortness of breath or pain in your jaw or arm. You should also go to the ER if you have bloody stools or vomit that looks like coffee grounds, which are signs of bleeding in the stomach.
Editor Lindsay Donaldson contributed to this article.
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.

