Ulcerative Colitis
Ulcerative colitis is a chronic disorder of the digestive system affecting the large intestine. People with this condition experience abnormal inflammation resulting in open sores called ulcers inside the colon and rectum.
Ulcerative colitis, or UC, is the result of an overactive immune system. The ulcers created in the large intestine produce mucus and pus which may cause abdominal pain in some people. People with this condition typically have frequent diarrhea. An estimated 750,000 people in North America are affected by UC.
Other names for the condition include colitis gravis, idiopathic proctocolitis and inflammatory bowel disease, ulcerative colitis type.
It is a long-term condition that can develop at any age, but most people are diagnosed between the ages of 15 and 30.
Family genetics also play a role in whether some people develop ulcerative colitis. The risk of developing it is between 1.6 percent and 30 percent if you have a close relative with it, according to the Crohn’s & Colitis Foundation.
Ulcerative colitis usually begins gradually but gets worse over time. It can go into remission, however, allowing symptoms to disappear for weeks or even years.
People with ulcerative colitis may benefit from care by a medical specialist called a gastroenterologist — a doctor specializing in digestive tract diseases and treatment — to manage their condition and improve their overall health. With proper treatment, people with UC can improve their quality of life.
What Causes Ulcerative Colitis?
Autoimmune disorders are not fully understood and the medical community isn’t quite sure exactly how a person gets ulcerative colitis. But doctors and researchers have found that a variety of genetic and environmental factors may play a role in the case of UC.
Genetic Causes
Ulcerative colitis seems to run in some families. Studies have identified variations in genes that may play a role in causing UC, but researchers aren’t sure exactly how these genetic differences are directly linked to the condition.
Overactive Intestinal Immune System
The immune system protects the body by reacting to harmful invaders such as viruses, bacteria and other threats. Researchers believe these invaders may confuse the immune system, tricking it into launching an immune response in the lining of the large intestine, causing UC.
Environmental Causes
Most research suggests environmental factors may increase the chance of developing ulcerative colitis, but believe the risk is low. High-fat diets may trigger UC in some people. Individuals may notice specific foods cause a reaction for them.
Some drugs may also increase a person’s risk. Nonsteroidal anti-inflammatory drugs (NSAIDS) such as aspirin, ibuprofen (Advil and Motrin), naproxen (Aleve) and Celebrex may increase a person’s risk. Anti-acne drug Accutane has been blamed for increased UC risk. Antibiotics and oral contraceptives are also suspected of slightly increasing a person’s ulcerative colitis risk.
Emotional Stress
Emotional stress does not appear to cause ulcerative colitis. But some studies suggest that it can trigger a flare-up in some people after they’ve developed UC.
Ulcerative Colitis Symptoms
About half the people with ulcerative colitis experience only minor symptoms and symptoms may vary from person to person. But about 10 percent of people with the condition can have severe symptoms.
- Urgent and loose bowel movements
- Bloody stool
- Abdominal cramps, discomfort or pain
- Persistent diarrhea with blood, pus or mucus in the stool
- Nausea
- Loss of appetite
- Fatigue
- Fever
- Anemia due to excessive intestinal bleeding
- Weight loss
- Slowed or delayed growth in children
Source: National Institutes of Health
Less common symptoms may include eye irritation, joint pain or soreness and rashes, according to the National Institutes of Health.
Types of Ulcerative Colitis
There are five types of ulcerative colitis that are identified largely by where they are located in the body or their severity. Symptoms differ between each type of UC.
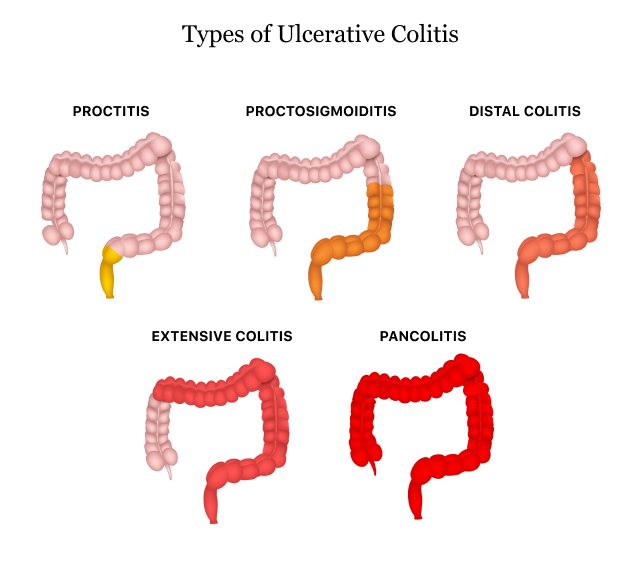
Ulcerative Procitis
This is usually the mildest form of UC. It is limited to the rectum and rectal bleeding may be the only sign or symptom.
Proctosigmoiditis
This type affects the lower end of the colon along with the rectum and is sometimes called sigmoid colon. Symptoms include bloody diarrhea, abdominal cramps and pain.
Left-Sided Colitis
This type causes cramps on the left side of the abdomen affecting the rectum and the portion of the colon on the left side of the body. Signs and symptoms include bloody diarrhea and weight loss.
Pancolitis
Pancolitis can affect the entire colon, causing multiple symptoms including bloody diarrhea, major weight loss, pain, fatigue and abdominal cramps.
Acute Severe Ulcerative Colitis
This condition is rare but affects the entire colon. Symptoms include bloody diarrhea, pain and fever.
What’s the Difference: Crohn’s Disease vs. Ulcerative Colitis
Crohn’s disease and ulcerative colitis are different medical conditions related to digestive health. But they are both inflammatory bowel diseases (IBDs). Microscopic colitis is another common IBD.
Ulcerative colitis affects only the inner surface of the colon. Crohn’s disease can cause inflammation in any part of the digestive system from the mouth through the rectum. Crohn’s disease also causes swelling and pain deeper into the tissue of the large intestine.
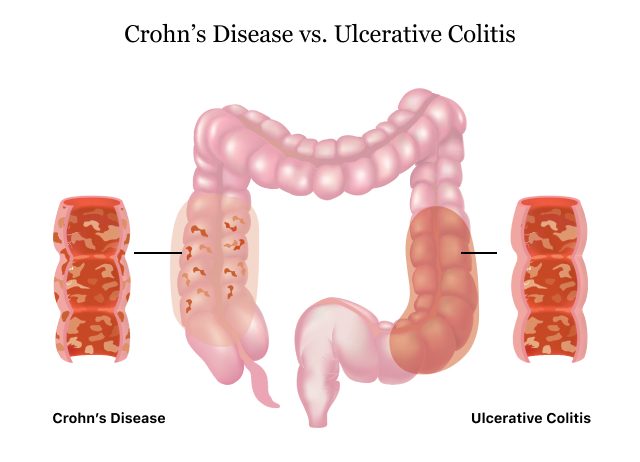
The term colitis applies to the swelling or inflammation of the colon — the large intestine. With microscopic colitis, the inflammation can only be seen with a microscope. Ulcerative colitis causes much larger swelling.
Diagnosing and Treating Ulcerative Colitis
There are four ways to diagnose ulcerative colitis. It is usually treated through medications or surgery.
- A review of the patient’s family history of UC
- Physical exam to check for swelling, listen for sounds in the abdomen, and check for tenderness or pain in the abdomen
- Lab tests of blood and stool that check for anemia, inflammation elsewhere in the body and other markers common to UC patients
- Use of an endoscope, a long, flexible tube with a camera, to look at the colon
Source: National Institutes of Health
Treatment options depend on the severity of the patient’s ulcerative colitis. Surgery may require removing the colon and rectum in the most severe cases.
Medications for Ulcerative Colitis
No medicine can cure UC. The goal of medication is to make a patient’s ulcerative colitis manageable. People with UC may have to take medicines indefinitely to control their condition.
- Aminosalicylates
- These medications may be used in people with mild or moderate symptoms and most people can tolerate them. They contain an active ingredient called 5-aminosalisylic acid, or 5-ASA, which helps control inflammation. Drugs in this class include balsalazide, mesalamine, olsalazine and sulfasalazine.
- Corticosteroids
- More commonly known simply as steroids, these medicines reduce the immune system’s response. They are used if aminosalicylates don’t seem to work. Drugs in this class include prednisone, methylprednisone, hydrocortisone and budesonide. These drugs shouldn’t be used long-term.
- Immunomodulators
- These drugs reduce immune system activity as well, but may take as long as three months to work. Immunomodulators include Azasan or Imuran (azathioprine) and Purinethol or Purixan (6-mercaptopurine).
- Biologics or TNF therapy
- This group includes Humira (adalimumab), Simponi (golimumab) and Remicade (infliximab), medications that decrease inflammation by targeting a protein made by the immune system called tumor necrosis factor, or TNF. Side effects of these medications include higher risks for tuberculosis, fungal infections, skin cancer and psoriasis.
In the past, Xeljanz and Xeljanz XR (tofacitinib) were used to treat ulcerative colitis. These drugs work in a different way from anti-TNF drugs to treat UC. But the U.S. Food and Drug Administration limited the drugs’ use in 2019 due to safety concerns. They are now only approved for use in adults with UC who are unable to tolerate or have an inadequate response to treatment with TNF therapy.
Health care providers may also use other drugs such as Tylenol (acetaminophen) to treat mild pain. People with UC should avoid using Advil or Motrin (ibuprofen), Aleve (naproxen) and aspirin because they can make symptoms such as bleeding worse.
Doctors may also recommend antibiotics to prevent infection and other medications to treat diarrhea.
Colon Cancer and Other Ulcerative Colitis Complications
The most serious complication of ulcerative colitis can be colon cancer. This is more likely to occur in people who have had UC for eight or more years and in people who have inflammation through the whole colon.
People with UC should talk with their health care provider about scheduling recurring cancer screenings. People with ulcerative colitis may need colonoscopies every one to three years if they have UC in more than a third of their colon or have had the condition for eight years or more.
Another life-threatening but rare complication is toxic megacolon. It involves the widening of the colon and an overwhelming bacterial infection resulting in sepsis. Sepsis is the body’s extreme reaction to an infection. It can lead to tissue damage, organ failure and death according to the U.S. Centers for Disease Control and Prevention.
- Rectal bleeding leading to anemia
- Dehydration and malabsorption if the colon is unable to absorb fluids and nutrients
- Bone changes such as osteoporosis (bone loss) or osteopenia (low bone density)
- Inflammation to other parts of the body such as the joints, eyes, skin or liver
How Eating, Diet and Nutrition Affect Ulcerative Colitis
Eating, diet and nutrition all play a role in causing ulcerative colitis symptoms. People with UC should talk with a healthcare provider about changes to their diet.
- Carbonated drinks
- Popcorn
- Vegetable skins
- Nuts
- High-fiber foods (when symptoms are present)
Source: National Institutes of Health
Doctors may recommend that people with UC drink more fluids, eat more frequent but smaller meals, and keep a food diary to track the particular foods that may cause problems. It’s important to try to eat a balanced diet because it plays a big role in the health of your immune system. An estimated 70 percent to 80 percent of immune cells live in the gut.
No one diet is recommended for all patients, as different foods can trigger UC symptoms in different patients. Your health care provider can help you find a diet that is right for you.
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.

