
Interstitial Cystitis
Interstitial cystitis (IC), also known as bladder pain syndrome, is a chronic condition characterized by persistent bladder pain, discomfort and an urgent need to urinate. Symptoms can range from mild irritation to debilitating pain. There is no definitive cause and no cure, but you can manage your IC symptoms.

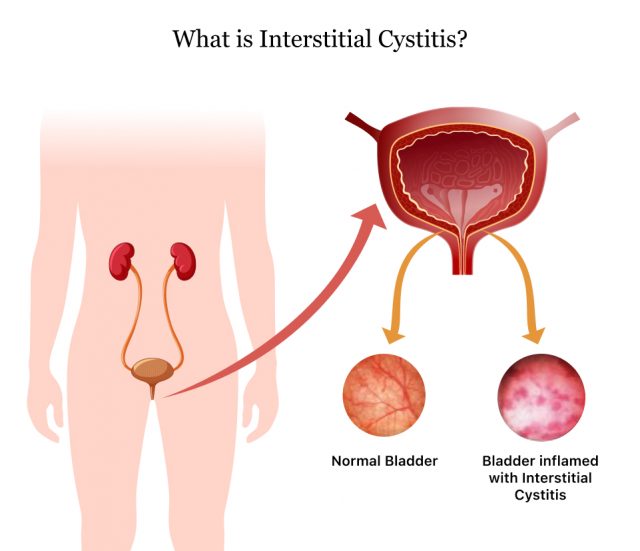
What Is Interstitial Cystitis?
Interstitial cystitis (IC), also called bladder pain syndrome, is a chronic condition that causes discomfort or pain in the bladder and pelvic region. People with IC may feel a constant need to urinate, even when their bladder isn’t full. They might experience frequent urination along with pressure or chronic pain.
Symptoms vary from mild discomfort to severe pain. While the exact cause of IC is unclear, experts believe it might indicate a more complicated systemic condition or disorder. These may include conditions such as inflammatory bowel disease, lupus, irritable bowel syndrome or fibromyalgia.
Some researchers also theorize that bladder wall defects, unusual immune responses, or nerve sensitivities cause IC.
IC can be difficult to manage, but treatments focus on reducing symptoms and improving quality of life. Sometimes, the condition can go into remission.
Symptoms of Interstitial Cystitis
The symptoms of interstitial cystitis are varied and may include pelvic pain, frequent urination and painful intercourse. The condition can sometimes cause mild discomfort or severe pain. The severity of symptoms can be unpredictable and make daily life difficult.
For people with IC, bladder pain and urinary issues become all too common. The symptoms can come and go, with intense flare-ups followed by some relief.
- An urgent need to urinate, even right after going
- Continuous pelvic pain, discomfort or pressure
- Frequent urination during the day and night
- Pain in the vulva, vagina, scrotum or penis during sex
- Pain or burning when the bladder is full (may improve after urination)
Interstitial cystitis (IC) affects about 1% of people in the U.S., with women being nearly twice as likely as men to develop it. If you experience persistent bladder pain, frequent urination or an urgent need to pee, seek medical treatment.
Many conditions, such as urinary tract infections, present similar symptoms to IC but require different treatment. A correct diagnosis can help you manage your pain and prevent it from getting worse.
What Causes Interstitial Cystitis?
IC may result from issues affecting the bladder, immune system and nerves. However, the exact cause of interstitial cystitis (IC) is unknown.
- Autoimmune Response
- Autoimmune responses where the body mistakenly attacks the bladder, leading to inflammation
- Bladder Damage
- Damage to the bladder's protective lining may allow substances in the urine to inflame the bladder wall
- Diet
- Certain foods and drinks — such as coffee, chocolate and alcohol — can trigger or worsen symptoms
- Genetics
- Genetic predisposition can increase your risk
- Nerve Problems
- Nerve problems can cause increased sensitivity and pain
- Urinary Tract Infections
- Frequent or chronic infections of the urinary tract
These factors can contribute to IC, making it a complex condition to diagnose and treat.
Medications That May Cause or Exacerbate Interstitial Cystitis
It’s unclear if any medications cause or worsen interstitial cystitis, but non-steroidal anti-inflammatory drugs (NSAIDs) may exacerbate bladder problems.
People with interstitial cystitis often use NSAIDs, like ibuprofen and aspirin, to treat pain from IC. However, long-term use of these drugs can increase fluid retention. You may urinate more frequently as your body tries to get rid of the extra fluid.
Diagnosing Interstitial Cystitis
IC is diagnosed through a process of elimination, because there isn’t a specific test for it. Doctors start by checking for other possible health conditions before diagnosing IC.

For the diagnosis, your health care provider may ask about your medical history, conduct a physical exam and test your urine. Sometimes, they use a tiny camera to look inside the bladder for any issues. Once they rule out other conditions, they can diagnose IC and start treatment. The treatment is often based on your specific symptoms.
Medications Used to Treat Interstitial Cystitis
Because no cure exists, interstitial cystitis (IC) treatment typically involves medications to alleviate symptoms. Doctors may recommend several drug treatment approaches.
- Elmiron (pentosan polysulfate sodium)
- Elmiron is the only FDA-approved oral medication specifically for IC. It forms a protective layer on the bladder wall to prevent irritation. Elmiron side effects include stomach pain, nausea and diarrhea. In addition, long-term use may be associated with vision problems, including pigmentary maculopathy. This condition can lead to vision loss.
- Elavil (amitriptyline)
- This is a low-dose antidepressant that helps reduce pain by altering pain perception. Side effects of amitriptyline include drowsiness, dry mouth and weight gain. The medication’s benefits typically become noticeable after several weeks.
- Dimethyl sulfoxide (DMSO)
- This is another FDA-approved drug, but doctors administer it directly into the bladder via a catheter. DMSO relieves IC symptoms, although it can cause discomfort during administration. It may also cause a garlic-like odor on your breath and skin.
- Antihistamines & NSAIDs
- Some doctors recommend using antihistamines like hydroxyzine and over-the-counter pain relievers like ibuprofen to help with the symptoms of interstitial cystitis. It's common for patients to need a combination of medications to get relief.
Case Study: Successful Treatment of IC with Singulair
Interstitial cystitis affects women more often than men. Its symptoms are similar to those of urinary tract infections (UTIs) and overactive bladder. For the 26-year-old woman profiled in a 2018 Cureus case report, the journey to understanding her chronic bladder pain led to an unexpected treatment.
The woman sought help after experiencing lower abdominal pain and an increase in urinary frequency for seven months. She reported urinating 20 to 35 times during the day and waking up six to eight times at night. Her pain level fluctuated, reaching a six out of 10. After tests and imaging, including an ultrasound and cystoscopy, doctors ruled out other causes. They then diagnosed her with IC.
The patient also had asthma and experienced a flare-up during her hospital stay. After receiving treatment for her asthma, doctors prescribed Singulair (montelukast). Montelukast is a medication commonly used to manage allergies and asthma. Soon after starting montelukast, the patient saw a big improvement in her urinary symptoms and pelvic pain.
Two months later, the patient reported dramatic improvements at a follow-up appointment. Her urinary frequency and pain had nearly disappeared. The report’s authors said this case highlights the potential of Singulair as an effective treatment for interstitial cystitis, especially in patients with a history of allergies or asthma.
The authors suspect montelukast may improve IC because it inhibits the receptors that activate mast cells. Mast cells are immune cells that are often overactive in the bladders of people with IC, causing inflammation.
Other Treatments for Interstitial Cystitis
Managing interstitial cystitis (IC) often requires more than simply relying on medications. Non-medication methods can also help address the physical and behavioral factors causing symptoms.
- Bladder instillations
- Your health care provider may administer medications like DMSO through a catheter. They may also use a combination of drugs, such as lidocaine and heparin. Doing this regularly may help repair the bladder walls and decrease the sensitivity of your bladder nerves.
- Bladder training (timed voiding)
- Gradually increasing the time between bathroom visits can help the bladder hold more urine. This may reduce the frequency of having to urinate. You can do bladder training by increasing the time you typically wait between urinations by 15 minutes. Each week, add another 15 minutes to the wait time. Because people typically urinate every 3-4 hours, you should aim for at least 2.5 hours between urinations.
- Botulinum toxin injections
- Injecting botulinum toxin into the bladder wall helps it relax and reduces pain. The effects typically last about six months, so repeated treatments are often necessary.
- Cystoscopy with hydrodistention
- This procedure involves examining the bladder with a telescope and stretching it to its maximum capacity. When the bladder is stretched out, it becomes easier to see the entire inner surface. Cystoscopy can help locate bladder lesions for treatment, temporarily relieving symptoms.
- Electrical stimulation (sacral nerve stimulation)
- Doctors perform surgery to embed a wire and pulse generator under the skin near the tailbone. This generator sends electrical pulses that stimulate sacral nerves and disrupt pain signals. This method is used when other treatments fail. However, it carries the risk of infection. Further surgery to reposition the device is also often required.
- Pelvic floor physical therapy
- Physical therapists release tension in the pelvic muscles, reducing bladder pain and improving urinary symptoms. Therapy usually takes place weekly over several months and includes exercises, like Kegels, that you continue at home.
These methods can significantly alleviate pain, reduce urinary frequency and enhance bladder control. Combining these treatments may yield improved outcomes for individuals with IC.
Lifestyle Considerations
Managing your daily habits, diet and stress is essential to reducing flare-ups and feeling better. Living with interstitial cystitis (IC) involves a variety of treatments.
Identifying and avoiding triggers and making targeted changes can help your bladder health and ease your symptoms.
- Diet Adjustments
- Managing interstitial cystitis may involve changing your diet. This means avoiding beverages that include citrus, caffeine or alcohol, which can worsen symptoms. Following an elimination diet to track which foods make your symptoms worse can help you take control of your diet and feel better.
- Increase Water Intake
- Increasing water intake is a simple yet effective strategy for managing IC. It helps make urine less acidic, thereby reducing irritation during flare-ups.
- Leverage Online Resources
- Websites like the Interstitial Cystitis Network provide helpful information, community support and resources for people with IC.
- Stress Management
- Stress can worsen the symptoms of IC. Relaxation methods like meditation or deep breathing can help you overcome your stress and feel more in control of your symptoms.
- Use Acid Reducers
- Over-the-counter supplements like Prelief can reduce the acidity of meals, potentially preventing flare-ups.
- Wear Comfortable Clothing
- Avoid wearing tight clothes that put pressure on your lower belly. Instead, wear looser jeans or adjust your clothes to feel more comfortable and reduce pressure on your waist and pelvic region.
Many IC patients significantly improve their symptoms by making these lifestyle adjustments. Your doctor can also help you develop a coordinated plan to live with this chronic condition.
Editor Lindsay Donaldson contributed to this article.
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.

