Maculopathy (Macular Degeneration)
Maculopathy, or macular degeneration, causes gradual vision loss in the center of your sight, making everyday tasks harder. While some drugs, like anti-VEGF treatments, can slow its progression, others may increase the risk of developing or worsening this eye condition.

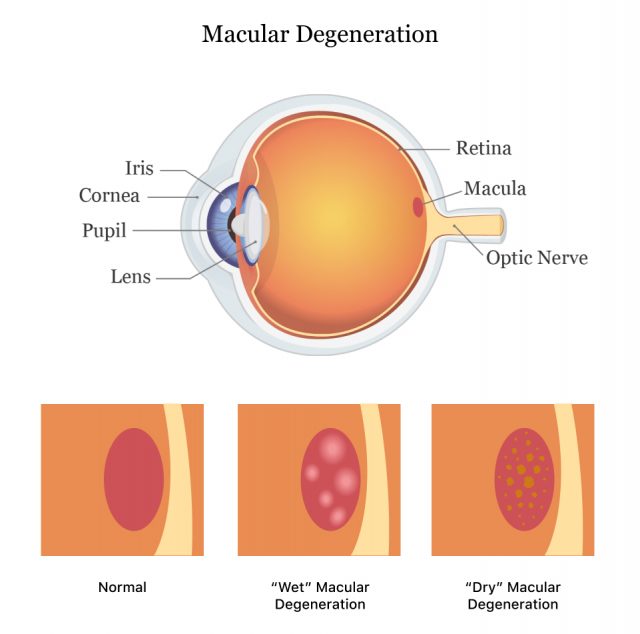
What Is Maculopathy?
Maculopathy, also known as macular degeneration, refers to a group of disorders that affect the central vision. It occurs when a part of the retina, called the macula, starts to break down. This condition causes the gradual loss of someone’s ability to see what’s right in front of them. It can make reading, driving and recognizing faces more challenging.
Those with maculopathy still have peripheral vision, so they can see what’s on either side of them. It can affect one or both eyes, and one may be affected more than the other.
While there isn’t a cure for macular degeneration, early intervention can slow its progression or reduce its severity.
Types of Maculopathy
Macular degeneration is divided into two categories: dry and wet. Both are more common in older adults.
Dry Macular Degeneration
Dry (atrophic) maculopathy occurs when your center of vision gradually and painlessly disappears in one or both eyes. It happens when the cells that allow you to sense light die and are not replaced.
In dry maculopathy, vision loss can begin in one or both eyes. If both eyes are affected, they may not have identical vision loss.
According to the Cleveland Clinic, around 90% of people with maculopathy have dry macular degeneration.
Wet Macular Degeneration
Wet maculopathy is a rare consequence of dry macular degeneration. In this condition, abnormal blood vessels grow under the retina, leading to leakage and scarring. Symptoms typically start suddenly and worsen rapidly.
A sudden loss of vision from dry or wet maculopathy may cause hallucinations, though it’s more common with wet maculopathy. Vision loss may be total, but early intervention can help.
This form of maculopathy only affects about 10% of people with macular degeneration.
Macular degeneration includes several specific diseases and disorders within the larger categories of wet and dry maculopathy.
- Age-Related Macular Degeneration (AMD)
- Age-related macular degeneration (AMD) is the most common reason older people lose central vision. It comes in two forms: dry (gradual thinning of the retina) and wet (abnormal blood vessel growth leading to leakage and scarring).
- Myopic Maculopathy
- Myopic maculopathy (MM) is a leading cause of severe nearsightedness. With nearsightedness, people struggle to see distant things clearly. People with MM have longer-than-average eyes, leading to sclera (white outer coating of the eye) and retina thinning. Family history is a significant risk indicator for myopic degeneration.
- Diabetic Macular Edema
- Diabetic macular edema (DME) is similar to wet maculopathy because they're both retinal vascular diseases. DME, however, involves damage to existing blood vessels, while wet macular degeneration deals with blood vessel growth. Some treatments may improve symptoms of both DME and wet macular degeneration.
- Hereditary or Genetic Maculopathies
- Between 15% and 20% of those with age-related macular degeneration likely have at least one immediate relative with AMD.
- Macular Pucker
- Epiretinal membrane, also called macular pucker or cellophane maculopathy, is when scar tissue on the retina blurs or distorts vision. This usually develops with age or other eye conditions.
- Macular Hole
- A macular hole forms when the jelly-like substance in the eye pulls away from the retina as you age. This is usually harmless, but a hole can form if it gets stuck on the retina as it pulls. Then, a dark or blind spot may appear.
Macular Degeneration Symptoms
Macular degeneration can creep up on you without early symptoms. Because the macula sends visual information from your eyes to your brain, damage to it disrupts your image perception.

Macular degeneration includes several specific diseases and disorders within the larger categories of wet and dry maculopathy.
- Difficulty seeing objects straight in front of you
- Lowered ability to see things that are far away
- Blurred vision
- Colors appearing faded or different
- Dark or blank spots in your central field of vision
- Distorted vision, where objects appear deformed or shrunken (metamorphopsia)
- Straight lines appearing wavy or curved
- Trouble seeing in low light
What Causes Macular Degeneration?
The cause of macular degeneration isn’t totally understood, though age, injuries, genetics, health issues and other factors can indicate your level of risk.
- Being 50 years old or older
- Cigarette smoking/tobacco use
- Excessive alcohol consumption
- Excessive sun exposure
- Head injuries
- High blood pressure
- Lack of physical activity
- Diabetes
- Diet lacking key nutrients
- Family history of macular degeneration
- Obesity
Medications Used to Treat Maculopathy
Macular degeneration is a severe eye condition, but thanks to medical advances, treatments can slow its progression and, in some cases, even improve vision.
Treatments for Wet Macular Degeneration
Wet AMD has been treated with eye injections for years. Since about 2005, anti-VEGF (vascular endothelial growth factor) injections have helped slow, stop or even improve patients’ vision. Anti-VEGF injections slow the growth of abnormal blood vessels in the eye. These vessels might leak blood or other fluids without treatment, causing wet AMD.
- Avastin (bevacizumab)
- Originally used to treat cancer, Avastin is often used off-label to treat wet AMD. Like other anti-VEGF drugs, it stops the growth of abnormal blood vessels.
- Eylea (aflibercept)
- This medication blocks a protein that causes abnormal blood vessel growth. A newer version of this drug, Eylea HD, has a higher dose and can last up to 3 to 4 months between injections, making it more convenient for patients.
- Lucentis (ranibizumab)
- Another anti-VEGF drug, Lucentis (ranibizumab), also stops blood vessel growth. It’s injected into the eye to help stabilize or improve vision, though patients still need regular injections.
- Sozinibercept
- As of 2024, this combination drug from Opthea is in Phase 3 clinical trials. It seems to be more effective when used with other anti-VEGF treatments.
- Vabysmo (faricimab)
- This drug targets VEGF and angiopoietin-2, which are proteins that contribute to blood vessel growth. This drug helps reduce abnormal blood vessels and inflammation. It can last longer between injections, typically every 3 to 4 months.
Treatments for Dry Macular Degeneration
Dry AMD has long been treated by antioxidant vitamins, but late-stage dry AMD has only recently become treatable.
Antioxidants help reduce damage from free radicals, which are byproducts of our cells using oxygen to create energy. Because of the way it interacts with light, the retina tends to have more free radicals than other body parts. Too many free radicals can lead to age-related diseases, so antioxidants can help slow the progression of early-stage dry AMD.
- AREDS2 Formula
- This antioxidant vitamin supplement can help slow vision loss in people with intermediate dry AMD.
- Syfovre (pegcetacoplan) and Izervay (avacincaptad pegol)
- These drugs target a part of the immune system known as the complement cascade, which can damage the retina. They slow the progression of late-stage AMD (geographic atrophy) by up to 20%, but they don’t improve vision. Though they're very similar, they work on different immune molecules.
- Stem Cells
- Although not yet approved, using stem cells to replace cells that die during dry AMD is being attempted in small clinical trials.
Other Treatments for Maculopathy
While medications play a significant role in treating macular degeneration, they aren’t the only options available. Many treatments and lifestyle adjustments can help you slow down vision loss and, in some cases, even restore damaged cells.
- Laser Photocoagulation
- Laser photocoagulation treats wet AMD using focused light to burn and seal off abnormal blood vessels under the eye’s macula. It may bring back lost vision or slow degeneration. Risks can include scarring that may cause or worsen blind spots, bleeding in the eye or retinal damage that may appear immediately or years later.
- Lifestyle Adjustments
- You may be able to slow down dry macular degeneration by changing habits. Your doctor can help guide you in making beneficial lifestyle choices. Lowering your blood pressure, not smoking, eating healthfully and being physically active may all make a positive impact. Your doctor may also recommend taking supplements, such as the AREDS2 formulation designed for eye health, and wearing sunglasses and wide-brimmed hats to protect your eyes from the sun.
- Photodynamic Therapy (PDT)
- Photodynamic therapy (PDT) treats wet AMD using a laser and a light-activated drug. The drug, injected into a vein in your arm, accumulates in the abnormal blood vessels under your macula. After giving you an anesthetic eye drop, the doctor shines a laser into your eye, which causes the collected medicine to create blood clots. These clots may prevent further vision loss. Risks can include new blind spots, photosensitivity, reaction at the injection site and temporary loss of visual acuity.
- Assistive Devices
- High and low-tech items may help people with AMD in everyday life. Large-print reading materials, handheld magnifiers (like magnifying glasses) and digital clocks with large numbers have been available for a long time. More recently, products like text-to-speech software, telescopic devices allowing for detailed vision at a distance, phone talk functions and CCTV magnifiers have become more accessible to consumers.
Combined with medications, these options can provide a range of treatments to manage macular degeneration and preserve your quality of life.
Drugs That Can Cause Macular Degeneration
No medications directly cause macular degeneration. However, you could be at a higher risk of developing AMD or having your disease progress faster if you take certain drugs.
If you’re worried about your risk of MD, it’s essential to talk to your doctor before making any changes to your prescribed medications.
- Anticholinergic drugs
- A study in JAMA Ophthalmology found that using strong anticholinergic medications for at least three months might increase the chances of developing late age-related macular degeneration. This drug class includes Spiriva, Cogentin, Robinul and several others. Anticholinergic drugs treat conditions caused by involuntary muscle movements, such as Parkinson’s disease and overactive bladder.
- Calcium channel blockers
- A 2021 study in Acta Ophthalmologica found that the calcium channel blockers amlodipine (brand names Norvasc, Katerzia and Norliqva) and felodipine (Plendil) may be linked to an increased risk of wet age-related macular degeneration. Calcium channel blockers can help treat heart conditions such as high blood pressure and abnormal heart rhythms.
- Elmiron
- Elmiron (pentosan polysulfate sodium), a common treatment for interstitial cystitis, has been linked to retinal toxicity. In one study on Kaiser Permanente patients in Northern California, about 25% of people who used Elmiron for at least five years developed the side effect of retinal damage. This damage can resemble macular degeneration. If not detected early and managed appropriately, it could lead to significant vision loss.
- Tamoxifen
- Tamoxifen (brand names Nolvadex and Soltamox), a medication often used for treating breast cancer, can cause eye problems, especially damage to the center of the retina. A 2024 study published in Nature found that around 12% of people who take it daily for over two years might experience eye changes, such as fluid buildup and crystal deposits.
If you take any of these medications and are concerned about MD, discussing the risks with your doctor is important.
Preventing Macular Degeneration
Several proactive strategies, such as having regular eye exams and maintaining a healthy diet and weight, can lower your risk of developing AMD and promote overall eye health.
Macular degeneration, particularly age-related macular degeneration, is a leading cause of vision loss in older adults. As maculopathy progresses, it can significantly affect daily tasks like reading and driving. Advanced maculopathy may lower your quality of life.
However, by making informed lifestyle choices and staying vigilant about your eye care, you can significantly enhance your chances of preserving your vision.
- Consider Supplements
- Daily intake of vitamins C and E, beta-carotene, zinc and copper may slow AMD progression.
- Eat a Nutritious Diet
- Focus on a diet rich in fruits, vegetables and fish. Antioxidants are particularly beneficial because they can help reduce retinal damage from light and lower cholesterol.
- Maintain a Healthy Weight
- Eat healthfully and exercise regularly as recommended by your physician.
- Manage Health Conditions
- Treat cardiovascular and other health issues with the assistance of your healthcare provider.
- Quit Smoking
- If you smoke, seek support to quit; smokers are at a higher risk for AMD. If you don’t smoke, don’t start.
- Regular Eye Exams
- Schedule routine check-ups to catch early signs of AMD.
By prioritizing eye health through these lifestyle changes, you can significantly lower your risk of macular degeneration. Early detection and prevention are your best defenses against maculopathy.
When to Seek Medical Attention
If you experience symptoms such as loss of central vision, it’s essential to seek medical attention immediately. Signs of central vision loss include noticing missing words while reading or a gray spot in your vision. Recognizing the signs of macular degeneration is crucial for maintaining eye health, as early detection can significantly impact treatment outcomes.
Wet macular degeneration, the more severe form, can cause sudden distortion in your central vision, making straight lines appear bent. Early intervention is vital because this progression can lead to substantial vision loss.
Amsler Grid Test and Diagnosing Macular Degeneration
The Amsler grid is a simple tool that helps detect early vision changes in people with age-related macular degeneration (AMD). It looks like a square with a central dot. You cover one eye, focus on the dot, and look at the grid. If the lines appear wavy, blurry, dark or have blank spots, it could mean your vision is changing because of AMD.
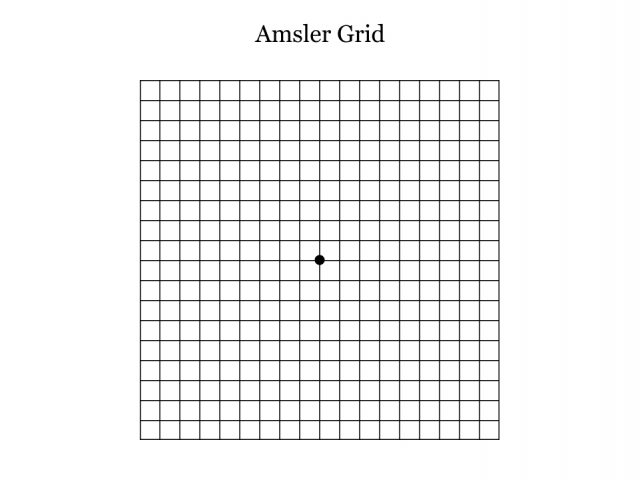
- Wear the glasses that you usually use to read.
- In good light, hold the grid 12 to 15 inches away.
- Cover one of your eyes.
- Keep your uncovered eye focused directly on the center dot.
- Without moving your focus from the dot, see if the lines on the grid are wavy, blurry, dark or blank.
- Repeat the steps with your other eye.
Using the grid daily can help you track any changes, especially if your AMD worsens. If you notice these problems early, contact your eye doctor right away.
Fully diagnosing macular degeneration typically involves a comprehensive eye examination.
- Dilated Eye Exam
- Eye drops widen your pupils, allowing for a thorough examination of your eye's interior.
- Fluorescein Angiography
- A dye is injected into your arm, revealing any blood vessel leakage in the eye.
- Optical Coherence Tomography (OCT)
- This imaging test captures detailed pictures of your retina and macula, providing crucial information for diagnosis.
It’s essential to have regular eye check-ups because sometimes you might not realize you have eye problems. When you go for an eye exam, the doctor will check if you need glasses or contact lenses. They will also make sure your eyes are healthy by looking at the back of your eyes to check for any issues with your retina and macula.
Editor Lindsay Donaldson contributed to this article.
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.


