Psoriasis
Psoriasis is a chronic autoimmune disease that causes skin cells to grow too fast, leading to sore, itchy, thick patches of red, scaly skin. It can happen anywhere on the body, but it usually affects the knees, elbows, back, scalp, palms and feet.

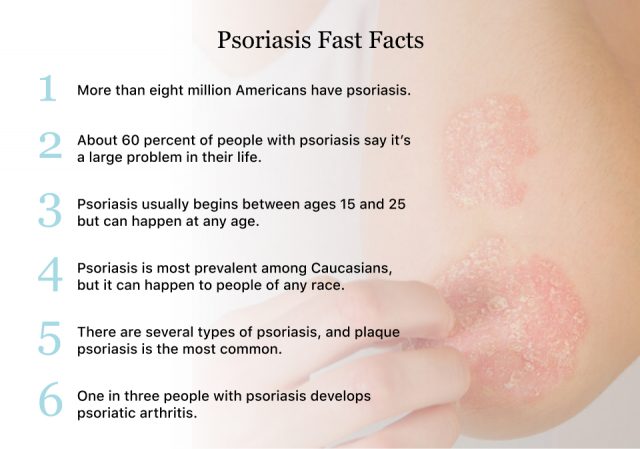
Psoriasis is a common disease, and more than eight million Americans have it, according to the National Psoriasis Foundation.
Psoriasis comes and goes in spurts. When the disease is active, it is called a flare. Flares can last for weeks or months and then go into remission or subside. Manifestations of the disease range from a few spots of scaly skin that resemble dandruff to more severe flare-ups that cover bigger areas of the body.
It’s not contagious, but it’s more than a cosmetic problem. About 60 percent of people with psoriasis said the disease interferes with their daily lives.
There is no cure for psoriasis, but people with psoriasis have treatment options aimed at controlling symptoms. Common treatments include light therapy (phototherapy), ointments, and medications.
What Are the Signs and Symptoms?
Psoriasis signs and symptoms vary from person to person. Depending on the type and severity of the disease, it may manifest differently.
People with psoriasis are also more likely to have co-occurring health conditions, including cardiovascular problems, obesity, high blood pressure and diabetes.
- In children, smaller, scaly spots
- Nails that are thick, ridged or pitted
- Pain, swelling or warmth
- Patches of red skin with thick, silvery scales
- Scaly scalp
- Skin that is dry and cracked, sometimes it itches or bleeds
- Soreness, burning or itching
- Stiff and achy joints
How Serious Is It?
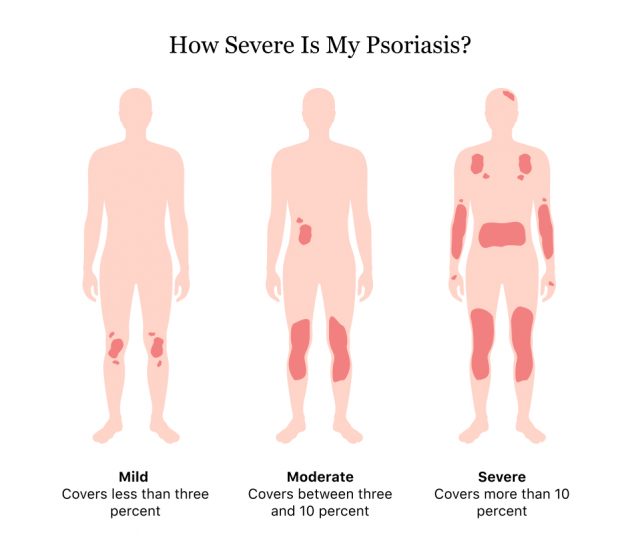
Psoriasis can be mild, moderate or severe depending on the percent of body surface area affected. The scale goes from less than three percent to over 10 percent.
For reference, a hand is about the same as one percent of skin surface, according to The National Psoriasis Foundation. How a person’s quality of life is affected is also a factor in classifying disease severity.
What Causes It?
Scientists don’t know exactly what causes psoriasis, but they know it’s an autoimmune disease. This means the body’s immune system overreacts, causing other health problems.
Immune cells called T cells become overactive and trigger immune responses such as swelling and abnormally quick skin cell growth, according to the National Institute of Arthritis and Musculoskeletal and Skin Diseases.
In people without psoriasis, skin cells usually take about a month to go through their life cycle. But in people with psoriasis, it only takes a few days. These extra skin cells grow deep in the skin and rise to the surface, causing red, scaly patches.
A few factors can cause flares.
- Alcoholism
- Infections
- Pregnancy
- Reactions to some medicines
- Stress
- Things that damage the skin, including sunburns, scrapes or cuts
- Weather changes that cause dry skin
Is It Hereditary?
Research suggests that psoriasis is hereditary, meaning it runs in families. One in three people with psoriasis report having a family member with the disease.
A child with one parent with psoriasis has a 10 percent chance of also having it. If a child has two parents with psoriasis, the likelihood they will get the disease increases to 50 percent, according to the National Psoriasis Foundation.
Most of these types of disease are chronic, but not life threatening. The rarest type, called erythrodermic psoriasis, is a severe disease and is a medical emergency.
Types of Psoriasis
According to the National Psoriasis Foundation, there are five main types of psoriasis. Each type differs in severity and symptoms. Doctors will vary the treatment recommendations depending on the type.
Plaque Psoriasis
Plaque psoriasis is the most common form. It appears as patches of red, raised skin covered with a silvery buildup of dead skin. These patches most commonly affect the scalp, elbows, knees and lower back.
Guttate Psoriasis
Guttate psoriasis most often affects children or young adults. This type of psoriasis appears as small, red, scaly dots on the trunk, arms and legs. Strep throat infections are a typical trigger.
Inverse Psoriasis
Inverse psoriasis affects the body in places with skin folds such as behind the knee, in the groin or under the arm. Unlike plaque psoriasis, it typically appears red, shiny and smooth. People who have this type of psoriasis usually have it on more than one part of the body at the same time.
Pustular Psoriasis
Pustular psoriasis is a rarer type of psoriasis that manifests as red skin with pustules, or blisters, filled with non-infectious pus. It occurs most often on the hands or feet, though it can occur anywhere on the body. The liquid in the blisters is made of white blood cells, and despite how it looks it is not an infection nor is it contagious.
Erythrodermic Psoriasis
Erythrodermic psoriasis is a very severe, but rare form of the disease. Only about three percent of people with psoriasis have this type. It causes extreme, widespread redness over most of the body. Skin layers come off in sheets and cause severe itching and pain. It can also cause dehydration, body temperature changes, changes in heart rate and nail changes.
This is a medical emergency. Seek medical help right away if you think you have erythrodermic psoriasis because it can be life threatening.
Diagnosis & Treatment
Doctors diagnose psoriasis by examining the rash or lesions. He or she will look at the scales and plaques and where they appear on the body.
Sometimes, the doctor will take a skin sample and send it off to a lab, a procedure called a biopsy. This allows the doctor to rule out other skin disorders such as skin cancer.
Treatment for psoriasis includes topical therapy, phototherapy (light therapy) and medications. Sometimes, doctors may recommend a combination of treatments.
Topical Therapy
Topical therapies typically come in the form of creams, shampoos, lotions, gels or ointments applied directly to the skin.
- Calcineurin inhibitors, such as tacrolimus, reduce plaques and inflammation
- Coal tar comes in creams, oils and shampoos and reduces inflammation, scaling and itching
- Corticosteroids such as hydrocortisone, triamcinolone (Acetonide, Trianex), clobetasol (Temovate) control flares
- Salicylic acid shampoos reduce scaling on the scalp
- Vitamin D slows skin cell growth
Phototherapy (Light Therapy)
Phototherapy is the go-to treatment for moderate to severe psoriasis. The doctor may recommend it alone or with medications. This type of therapy exposes the skin to controlled amounts of artificial or natural light to control psoriasis.
The light source may be natural sunlight, also called heliotherapy. Artificial light techniques include UVB broadband and narrowband therapy, Psoralen plus ultraviolet A and targeted laser therapy.
Side effects include skin dryness, itchy skin, skin burns, freckles, increased sun sensitivity and increased skin cancer risk. Moisturizing regularly may help with itchiness and dryness.
Other Medications
Medications for psoriasis include immunosuppressants and biologic agents that suppress the immune system to prevent psoriasis symptoms. These drugs reduce the body’s ability to fight off infections and may cause damage to organs such as the liver and kidneys.
- Cyclosporine, a drug that treats severe psoriasis
- Deucravacitinib, a drug that treats moderate-to-severe plaque psoriasis
- Methotrexate, a drug that slows down skin cell grows and decreases inflammation
- Acitretin, a vitamin A derivative that is effective for pustular psoriasis but may cause hair loss, liver and bone problems as well as birth defects
- Biologic agents such as Enbrel (etanercept), Xeljanz (tofacitinib), Humira (adalimumab), Remicade (infliximab) and others that suppress the immune system are the most effective drugs for severe psoriasis. But they can increase the risk of infections and certain types of cancer.
Psoriasis vs. Eczema
Psoriasis and eczema both cause itchy, red skin and it can be difficult to tell these rashes apart. The biggest difference is that psoriasis is an autoimmune disorder, and eczema is not.
Psoriasis tends to have a milder itchiness, whereas eczema can be more intense. The places most commonly affected by psoriasis are the scalp, elbows, knees, buttocks and face. Eczema most often occurs on the inside of the elbows or the back of the knees.
The rash caused by eczema usually comes with fluid leaking through the skin, whereas psoriasis is a thicker plaque with dry scaling.
The best way to tell these two rashes apart is to see a dermatologist.
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.

