Stevens-Johnson Syndrome
Stevens-Johnson syndrome is a rare, life-threatening reaction. It causes your skin and mucous membranes to blister and peel. Medications like antibiotics or anticonvulsants may trigger it. People with weakened immune systems, infections or specific genetic factors could be at higher risk.
What Is Stevens-Johnson Syndrome?
Stevens-Johnson syndrome is a rare but severe disorder that can cause lesions on your skin and the moist inner lining of organs like your nose, lungs, mouth and stomach. These linings are known as mucous membranes. It may also result in severe eye issues.
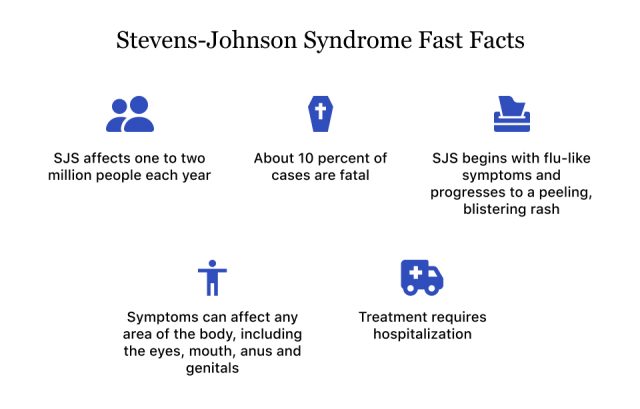
More than 80% of cases are linked to prescription or over-the-counter medications. An estimated two to seven million people are affected by Stevens-Johnson syndrome annually.
Stevens-Johnson syndrome may be mistaken for erythema multiforme major, a condition that also causes rashes and mucosal lesions. Stevens-Johnson syndrome is typically more serious, however, and may cause painful blisters and lesions on the face and torso. Erythema lesions are typically target-like in appearance, with a darker inner circle, and appear on the limbs.
You are more likely to develop Stevens-Johnson syndrome if you have a weak immune system, a family history of the disorder or take specific drugs like anticonvulsants or antibiotics. Infections and genetic factors can also play a role.
If you suspect you have Stevens-Johnson syndrome, seek medical help right away. It can cause severe complications like dehydration, sepsis, and vision problems.
Stevens-Johnson syndrome “is a potentially life-threatening condition, and much of the care is supportive,” Aaron Emmel, PharmD, board-certified pharmacotherapy specialist and founder of Pharmacy Tech Scholar, told Drugwatch. “This includes fluid replacement, nutrition support, skincare that may amount to the intensity of care that requires burn unit expertise, pain relief, respiratory support and infection prevention.”
Symptoms of Stevens-Johnson Syndrome
Stevens-Johnson syndrome symptoms typically begin with fever, headache, cough and body aches. These generally start one to three weeks after taking certain medications.
A flat red or purple rash may appear on your face, neck and body. This rash often spreads irregularly and forms painful blisters. Your mucous membranes may also be affected, resulting in sores in your mouth and eyes, making eating and opening your eyes painful.
This extensive damage can resemble burns and pose serious health risks.
Stevens-Johnson syndrome is a medical emergency. It needs hospitalization due to the risk of infections and organ damage.
What Is Toxic Epidermal Necrolysis?
Toxic epidermal necrolysis is a serious skin condition that occurs when Stevens-Johnson syndrome affects over 30% of your skin. Essentially, it is a more severe version of Stevens-Johnson syndrome. It can cause extensive skin peeling and sores in the body’s mucous membranes. It may lead to severe problems like infections and organ failure. People with this condition often need to be hospitalized in special units for intensive care and fluid management.
According to a 2023 article in StatPearls, Stevens-Johnson syndrome is three times more prevalent than toxic epidermal necrolysis.
Both toxic epidermal necrolysis and Stevens-Johnson syndrome are life-threatening. They require immediate medical attention. They can be caused by medications or infections and have similar symptoms, including fever and blisters.
Drugs That May Cause Stevens-Johnson Syndrome
Over 100 medications are associated with Stevens-Johnson syndrome, and some medications carry higher risk, Emmel said.
“Several anti-seizure medications, allopurinol, sulfonamides, several antibiotics and NSAIDs are examples of the medications that most commonly cause [Stevens-Johnson syndrome],” he said.
- Acetaminophen: Brand names include Tylenol. Acetaminophen is in scores of other medications, including Excedrin, Mucinex, Nyquil, Sudafed and Theraflu.
- Allopurinol: A prescription gout drug. The risk of Stevens-Johnson syndrome is particularly noticeable in Allopurinol doses over 100 mg per day.
- Antibiotics: Cephalosporins, minocycline, penicillins and quinolones
- Anticonvulsants: Carbamazepine, lamotrigine, phenobarbitone and phenytoin
- Contrast media: Substances used to improve the visibility of internal body structures in imaging techniques like CT scans, MRIs, ultrasounds and X-rays.
- Nevirapine: A non-nucleoside reverse-transcriptase inhibitor used to treat HIV.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): Oxicam-based NSAIDs, such as Meloxicam and Tenoxicam, are more likely to cause Stevens-Johnson Syndrome compared to NSAIDs such as Ibuprofen (Advil, Motrin) and naproxen (Aleve).
- Sulfonamides: Cotrimoxazole and sulfasalazine
Scientists are unsure how exactly medications cause Stevens-Johnson syndrome. But, according to a National Library of Medicine article, certain medications may cause the disorder in some people due to their genetic makeup. This could occur because of how their immune system reacts to the drugs.
Other Causes of Stevens-Johnson Syndrome
An allergic reaction to medication usually causes Stevens-Johnson syndrome. Genetics, infections and rare factors like vaccinations or graft-versus-host disease may also increase your risk.
Infections including pneumonia, herpes and hepatitis A have been connected to Stevens-Johnson syndrome. Mycoplasma pneumonia, specifically, is a notable cause.
People with weakened immune systems, like those with HIV, are at higher risk. Other concerns include a personal or family history of Stevens-Johnson syndrome, certain genetic variations and cancer, especially blood cancers.
Treatment for Stevens-Johnson Syndrome
Treatment for Stevens-Johnson syndrome and toxic epidermal necrolysis includes stopping the medication that caused the reaction and receiving care in specialized burn units or intensive care units.
“The biggest challenges in treating [Stevens-Johnson syndrome] include an accurate diagnosis and determining the offending medication,” Emmel said. “This requires a careful investigation, including comprehensive labs, skin biopsy and a complete history of the patient’s health status in the weeks leading up to the onset and the patient’s medication history.”
Preventing infection is a priority, and patients receive fluids and salts through an IV. While no specific treatment has been proven to increase survival, cyclosporine, an immunosuppressant, may reduce the duration of blistering and improve outcomes.
- Antibiotics (if there's an infection)
- Corticosteroids (to reduce damage from the immune system)
- Immunosuppressive drugs (to reduce damage from the immune system)
- Intravenous immune globulin (to regulate the immune system)
- Plasmapheresis (removing harmful substances from the blood)
“Another major challenge is a lack of definitive evidence on specific medical treatments for the syndrome itself,” Emmel said. “Corticosteroids, cyclosporine, etanercept, N-acetylcysteine and immune globulin therapies have all been utilized with some reports of effectiveness, but the evidence is inconclusive.”
With Stevens-Johnson syndrome, the chance of dying is lower than with toxic epidermal necrolysis, where the death rate is between 25% and 35% in adults. Children have a lower death rate from toxic epidermal necrolysis, ranging between 4% and 15%.
Patients typically do not need skin grafts as their skin grows back on its own. But, the conditions can still cause lasting problems, like itchy skin and a change in skin color. Additionally, if the rash had spread to the eyes, it could cause chronic eye issues. These eye problems include swelling, dry eyes and vision impairment.
Long-Term Management and Recovery
Recovery from Stevens-Johnson syndrome can take weeks to months. You may feel tired for weeks after leaving the hospital. While your skin typically heals within two to three weeks, it may take longer if a skin infection occurs.
To prevent Stevens-Johnson syndrome, you can get a genetic test for a specific gene variation called HLA-B*1502 before taking certain medications. People with Asian or South Asian heritage are more likely to have this gene.
If you’ve had Stevens-Johnson syndrome before, stay away from the medication that caused it. Your family members might need to avoid the medication as well.
Editor Lindsay Donaldson contributed to this article.
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.

