Sleep Apnea
Sleep apnea, a common sleep disorder, involves repeated pauses in breathing during sleep, leading to fragmented rest and serious health issues like heart disease and stroke. Treatment options like CPAP machines and oral appliances help manage sleep apnea and are crucial for better health.
What Is Sleep Apnea?
Sleep apnea is a disorder in which people experience reduced or paused breathing while asleep. These episodes, called hypopneas, last 10 or more seconds and occur several times throughout the night.
Obstructive sleep apnea (OSA) and central sleep apnea (CSA) are the two most common types of sleep apnea. Most patients with sleep apnea have OSA, which occurs when the airway becomes blocked. CSA happens when the brain doesn’t correctly tell the body to breathe.
Those with sleep apnea risk waking up their partners. Therefore, their partner may notice the symptoms first. Frequent sleep disruptions can cause fatigue and issues like heart disease, stroke and high blood pressure. Sleep apnea treatments include using breathing machines and oral devices, lifestyle changes and surgery.
Facts and Statistics About Sleep Apnea
Tens of millions of adults in the United States have sleep apnea diagnoses. Many others may have the disorder and be unaware of it. Treatment is essential, as sleep apnea can increase the risk of heart disease, stroke and more.
- An estimated 30 to 40 million U.S. adults have a sleep apnea diagnosis.
- About 936 million adults worldwide have obstructive sleep apnea (OSA).
- Snoring occurs in up to 94% of people with sleep apnea.
- Sleep apnea risk is higher for older adults, men, post-menopausal people and those carrying excess weight.
- Motor vehicle accidents are twice as likely among those with untreated sleep apnea.
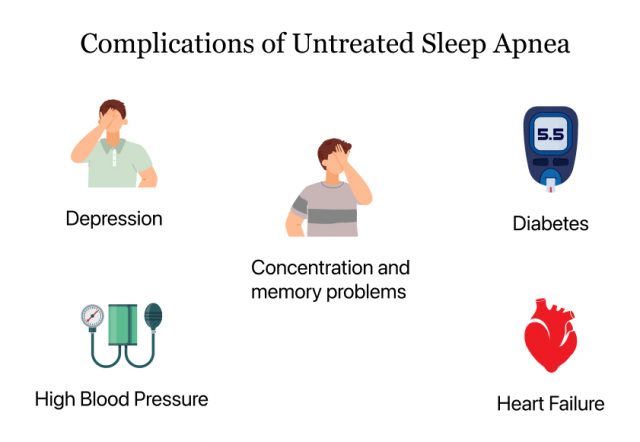
- Untreated sleep apnea is linked to high blood pressure, dementia, blood sugar issues, stroke and heart failure, among other serious health issues.
- It's believed that 33 million U.S. adults could benefit from CPAP treatment.
- Sleep apnea treatment may improve a patient's quality of life.
Types of Sleep Apnea and Their Causes
The primary types of sleep apnea are obstructive sleep apnea (OSA), central sleep apnea (CSA) and complex sleep apnea. OSA and CSA can occur naturally, with OSA being more common. Complex sleep apnea (also called treatment-emergent central sleep apnea) occurs when someone is treated for OSA but then develops CSA during this treatment. Fortunately, complex sleep apnea typically goes away after extended OSA treatment.
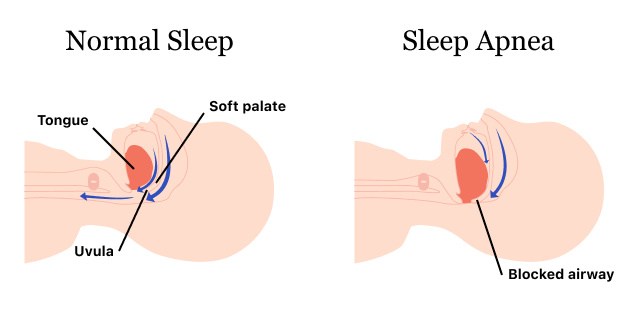
Obstructive Sleep Apnea
Obstructive sleep apnea occurs when the muscles at the back of the throat, which support several soft tissues, relax during sleep. This partially or totally closes the airway, lowering blood oxygen levels. These levels cause the brain to awaken the sleeper so breathing can resume. This can happen over a dozen times per hour, making restful sleep difficult to achieve.
Snoring is a significant symptom of OSA. It can also cause excessive sleepiness, morning headaches, difficulty focusing and mood changes. Severe issues like high blood pressure, heart disease and stroke can also occur.
OSA treatments can include the use of positive airway pressure, mouthpieces and surgery.
Central Sleep Apnea
Central sleep apnea is when the brain temporarily doesn’t signal the muscles that control breathing during sleep. CSA can be caused by congestive heart failure, stroke, the use of certain medications like opioids, sleeping at a high altitude or other issues.
Snoring can occur with CSA, but it isn’t necessarily a prominent feature of the ailment. Common symptoms include difficulty staying asleep, waking up short of breath and a partner noticing breathing pauses.
Addressing the underlying medical issues may treat CSA. A doctor may also prescribe a pressurized air system, supplemental oxygen or medication. In some cases, an electrical pulse directed at nerves or surgery may be recommended.
Sleep Apnea Symptoms
Sleep apnea symptoms vary from person to person and differ between OSA and CSA, but they always include breathing pauses periodically during sleep.
A lack of restful sleep caused by sleep apnea can result in difficulty functioning while awake. This can affect your health.
- Daytime sleepiness
- Difficulties with memory, focus and concentration
- Dry mouth or sore throat
- Erectile dysfunction and decreased libido
- Frequent loud snoring
- Frequently waking up
- Lower libido
- Loud snoring
- Morning headaches
- Pauses in breathing
- Tossing and turning while sleeping
- Unusual moodiness or irritability
CPAP and Related Machines
Positive airway pressure (PAP) machines like CPAP, BiPAP and APAP are often used to treat OSA. Oxygen therapy devices, which provide supplemental oxygen, may also be used.
CPAP Machines
A CPAP (continuous positive airway pressure) machine provides air pressure when you inhale and exhale. This prevents pauses in breathing and helps maintain steady breathing throughout the night.
CPAPs are the most commonly prescribed machine for those with OSA. However, if the pressure is too high, it can cause a choking sensation when you exhale. If turning down the pressure rate doesn’t help, you might consider trying an APAP or BiPAP instead.
APAP Machines
APAP can stand for automatic, auto-titrating, or auto-adjusting positive airway pressure. Unlike CPAP machines, which give you the same pressure all night, APAP machines adjust air pressure based on changes in breathing.
Doctors can review transcripts from APAP machines to refine treatment plans. However, APAPs can be more expensive than CPAPs, and not all insurance plans cover them.
BiPAP Machines
A BiPAP (bilevel positive airway pressure) machine provides higher air pressure when breathing in and lower when breathing out. This can make it easier to exhale compared to other machines.
Your doctor may recommend a BiPAP machine if you can’t comfortably use a CPAP or have complicated sleep apnea or breathing patterns.
Insurance doesn’t always cover BiPAP machines, though documented proof that a regular CPAP machine didn’t work for you might help your case.
Which Machine Is Right for You?
Your doctor will evaluate your specific needs and may recommend CPAP, APAP or BiPAP based on your breathing patterns, overall health, lifestyle and ability to afford the device.
Generally, insurance won’t cover an APAP or BiPAP until CPAP use has proven ineffective. So, doctors typically prescribe CPAPs first to those recently diagnosed with sleep apnea.
Recall and Side Effects of Philips Respironics PAP Machines
Philips Respironics recalled over 15 million CPAP and BiPAP machines and ventilators in 2021. The company had manufactured these devices between 2009 and 2021. This recall was due to the breakdown of polyester-based polyurethane (PE-PUR) foam, which could release harmful particles and chemicals.
Using these machines could lead to headaches, asthma, inflammatory responses and even cancer.
By September 2023, over 100,000 adverse events related to these machines were reported to the FDA from around the world. These included 561 deaths.

In 2023, another Philips CPAP recall was issued for replacement devices because of issues with their serial numbers. These incorrect or duplicate serial numbers could impact the device’s programming and affect the effectiveness of the therapy.
Philips agreed to a $479 million settlement to compensate people who bought or rented the affected devices.
Oral Appliances for Sleep Apnea
Doctors may explore treatments besides positive pressure machines for sleep apnea based on your needs. Alternatives like oral appliances, surgery or nerve stimulation are common options.
Oral appliances are custom-made and fitted by dentists. These devices are put into the mouth to help keep the airway open without using pressurized air.
- Mandibular Advancement Device (MAD)
- A MAD attaches to the top and bottom teeth and pulls the lower jaw and tongue forward. This allows more air to flow to the back of the throat.
- Rapid Maxillary Expansion (RME)
- This device is used to treat pediatric OSA. It widens the hard palate, allowing more air to pass through the nose to the throat and lungs.
- Tongue Muscle Stimulation Device
- This uses electrical signals to strengthen the tongue muscles and prevent the airway from being blocked by excessive tongue relaxation during sleep.
- Tongue-Retaining device (TRD)
- Also called a tongue-stabilizing device (TSD), a TRD uses suction to hold the tongue in place. This can prevent airway blockage.
Oral devices may be a good option for people who find CPAP machines too cumbersome. Users report that oral appliances are easier to wear, transport and care for than a PAP machine. However, they may not work as well for severe cases of sleep apnea and can take some time to get used to.
Most people adjust to discomfort caused by oral appliance therapy within a few weeks. While long-term issues are unlikely to occur if your device fits properly, they may include bite changes, teeth movement or jaw problems.
Medications Used to Treat Sleep Apnea
Several medications may help alleviate sleep apnea symptoms, though the FDA has only approved one for treatment. In December 2024, the FDA determined that the weight-loss drug Zepbound (tirzepatide), combined with a healthy diet and exercise routine, can treat moderate to severe OSA in adults with obesity. This was based on data from a study published in the New England Journal of Medicine.
Over a year, the researchers found that people with obesity and severe sleep apnea experienced fewer interruptions in their breathing and better heart health. Some even improved so much that CPAP machine use may no longer be necessary.
Another drug with the active ingredient tirzepatide is the diabetes medication Mounjaro. Although only Zepbound has FDA approval for sleep apnea treatment, both these medications have similar side effects.
Common Mounjaro (tirzepatide) side effects include nausea, vomiting, diarrhea and reduced appetite. Serious risks include low blood sugar, pancreatitis, gallbladder issues and gastroparesis (stomach paralysis). It also carries a boxed warning for thyroid tumor risks.
Though the FDA has only approved Zepbound, other drugs might relieve sleep apnea symptoms.
- Ambien and Edluar (zolpidem tartrate): Help with sleep efficiency.
- Cafcit (caffeine citrate): A central nervous system stimulant for premature babies.
- Hetlioz (tasimelteon): A melatonin receptor agonist.
- Nuvigil (armodafinil) and Provigil (modafinil): Helps with daytime sleepiness.
- Sunosi (solriamfetol): Helps with excessive daylight sleepiness due to OSA or narcolepsy.
- Xyrem (sodium oxybate): A sedative to help sleep.
Medications That Can Cause Sleep Apnea
Certain drugs can cause central sleep apnea by affecting the brain’s control of breathing. While opioids are a common cause, other medications like sodium oxybate, baclofen and gabapentin can also trigger CSA. Stopping the medication may resolve the issue, but you should always talk with your doctor before stopping any medication.
- Antihistamines
- Some antihistamines, like Allegra (fexofenadine) and Zyrtec (cetirizine), can cause weight gain. This, in turn, may increase your risk of sleep apnea.
- Atypical antipsychotics
- Some atypical antipsychotics, such as Clozaril, FazaClo (both clozapine) and Zyprexa (olanzapine), used to treat schizophrenia can cause weight gain, increasing your risk of sleep apnea.
- Barbiturates
- Barbiturate toxicity can result in sleep apnea and other breathing challenges. These drugs cause drowsiness and can be used as sedatives or to help control seizures.
- Benzodiazepines
- Often prescribed for insomnia, benzodiazepines can cause breathing to become shallow and throat muscles to relax. They can also make waking difficult.
- Non-opioid medications
- These include Depakote (valproic acid) and Brilinta (ticagrelor). These medications can cause central sleep apnea (CSA) by acting on brainstem receptors.
- Opioids
- Opioids can cause respiratory suppression, which can lead to breathing problems while sleeping.
Other Treatments and Lifestyle Changes for Sleep Apnea
Surgery, nerve stimulation and lifestyle changes can significantly relieve sleep apnea symptoms. Like PAP devices, these aim to reduce airway obstruction and improve breathing during sleep. However, they don’t involve being hooked up to a pressurized air machine.
- Avoiding Alcohol and Sedatives
- Drinking alcohol and taking sedatives can make your breathing problems during sleep worse. Try not to have them before bedtime, and talk to your doctor about any medications you are taking.
- Changing Sleep Posture
- Sleeping on your side instead of your back can help prevent your airway from becoming blocked. However, it might not eliminate OSA symptoms.
- Mouth Exercises
- Exercises to strengthen mouth and throat muscles can make sleep apnea less severe. A provider trained in myofunctional therapy can help guide you through these exercises.
- Nerve Stimulation
- This involves a device that can help keep the airways open by stimulating the nerves that control the tongue muscles. The device has multiple components that are surgically implanted near your ribs and around the hypoglossal nerve that controls your tongue. This could be a good option for people over 22 who haven't found relief with CPAP. However, it's essential to know that all surgeries have risks.
- Regular Exercise
- Regular exercise can help improve symptoms of obstructive sleep apnea. It does this by strengthening your breathing muscles and improving your overall health.
- Surgery
- Sleep apnea surgery can help clear or fix throat, nose or mouth problems that make breathing hard. While it can improve some physical issues, there are risks, and you might still need to use a CPAP machine afterward.
- Weight Loss
- Losing weight can help reduce how often you stop breathing while asleep if you have sleep apnea. In severe cases, doctors might suggest weight loss (bariatric) surgery.
Changing your daily habits can be particularly helpful in managing sleep apnea, especially when you combine them with other treatments.
When to Seek Medical Attention for Sleep Apnea
See a doctor if you show signs of sleep apnea, like loud snoring, pauses in breathing during sleep or waking up gasping for air. Other signs include feeling overly tired, waking up with headaches or having difficulty focusing.
If you notice symptoms of a heart attack or stroke, which can be related to untreated sleep apnea, seek immediate emergency help.
Editor Lindsay Donaldson contributed to this article.
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.

