Taking Antibiotics Safely
Ask your medical provider or pharmacist about taking antibiotics safely, and always take them exactly as directed. Be sure to ask about drug side effects or possible interactions with other medications you may be taking. Take antibiotics for the prescribed time, even after you feel better and symptoms have subsided.

What Are Antibiotics?
Antibiotics are medications that treat bacterial infections. They come in capsules, chewable tablets, powders for liquid suspension, intravenous formulations, creams and ointments. Most are available only by prescription, though some topical creams and ointments may be available over the counter.
Antibiotics can treat bacterial infections of the ear, nose, throat, genitourinary tract and respiratory system. Each type of antibiotic’s effectiveness varies by bacteria strain, so a medical provider will choose the antibiotic that will work best for the specific infection.
According to the American Chemical Society, penicillin was one of the greatest advances in therapeutic medicine of the 1940s. Since then, researchers have developed several other antibiotics. New antibiotics, like Zevtera (ceftobiprole medocaril sodium for injection), which the FDA approved in April 2024, are still being created and marketed.
- Strep throat
- Sinus infections
- Ear infections
- Urinary tract infections
- Traveler’s diarrhea
- Skin infections
- Pneumonia
- Pink eye (bacterial conjunctivitis)
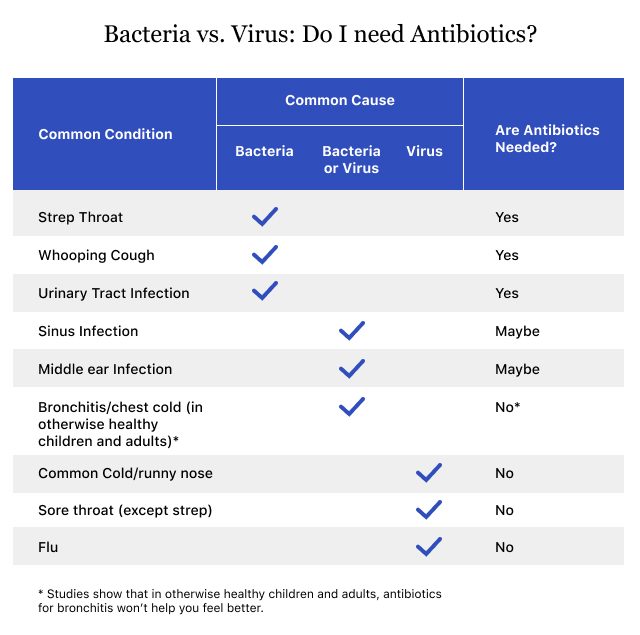
Antibiotics don’t work against infections caused by fungi, such as yeast infections and athlete’s foot, or viruses like the flu and the common cold.
Taking antibiotics responsibly is imperative. Misusing them, such as discontinuing use before the prescribed end date, can lead to a relapse of illness or antibiotic resistance, making it harder to treat severe infections down the line.
In 2024, a CDC report stressed the importance of doctors using caution when administering antibiotics, especially now that many medical visits can be conducted virtually.
The CDC has given more than $120 million to local health departments to help improve the use of antibiotics in doctors’ offices and hospitals when treating severe infections.

How Do They Work?
Generally, antibiotics work to treat bacteria in two ways. Some are bactericidal agents, which cause bacterial cell death, and others are bacteriostatic agents, which stop bacteria’s growth and reproduction.
For example, bactericidal antibiotics like penicillin and amoxicillin cause the breakdown of bacterial cell walls, which leads to cell death. Antibiotics like erythromycin and clarithromycin primarily prevent bacteria from synthesizing protein, stopping their growth.
According to Unity Point Health, antibiotics typically take action immediately, but it can take a few days to start feeling better. Each antibiotic stays in the body for varying lengths of time, but common antibiotics such as Amoxil (amoxicillin) and Cipro (ciprofloxacin) typically remain in your system for anywhere from 8 to 24 hours after the last dose. It can take longer for people with impaired kidney function to eliminate the drug from the body.
Some antibiotics, like Pfizer’s Zithromax or Z-Pack (azithromycin), stay in the body for about 15 days after the last dose.
Ask your pharmacist or medical provider how long your specific antibiotic stays in the body and other helpful information.

Common Types
Several classes of antibiotics are available in the United States. These drugs are grouped together by their chemical structure. Each class varies in effectiveness depending on the bacteria it’s treating.
| Class | Examples | How They Work |
|---|---|---|
| Beta-Lactams (sub classes: penicillins, carbapenems, cephalosporins, monobactams) | Penicillin, Amoxil (amoxicillin), Keflex (cephalexin), Premaxin (imipenem), Omnicef (cefdinir) | Kill bacteria by preventing formation of the bacterial cell wall |
| Fluoroquinolones / Quinolones | Cipro (ciprofloxacin), Levaquin (levofloxacin), Avelox (moxifloxacin) | Kill bacteria by preventing bacteria from making DNA |
| Macrolides | Zithromax, Z-Pak (azithromycin), Erythrocin (erythromycin) | Prevent bacteria from multiplying by preventing them from making proteins |
| Tetracyclines | Sumycin (tetracycline), Adoxa and Adoxa-Pak (doxycycline) | Prevent bacteria from multiplying by preventing them from making proteins |
| Glycopeptides | Vancocin (vancomycin), Dalvance (dalbavancin), Orbactiv (oritavancin) | Kill bacteria by preventing formation of the bacterial cell wall |
| Polypeptides | Baciim (bacitracin), polymyxin B | Kill bacteria by preventing formation of the bacterial cell wall |
| Sulfonamides | Sulfamylon (mafenide), sulfadiazine | Prevent bacteria from multiplying by preventing them from making proteins |
| Oxazolidinones | Zyvox (linezolid), Sivextro (tedizolid) | Prevent bacteria from multiplying by preventing them from making proteins |
| Nitroimidazoles | Flagyl (metronidazole), Tindamax (tinidazole) | Kills bacteria by disrupting production of genetic material |

How to Take Antibiotics
Always take antibiotics for the length of time that they are prescribed, even if symptoms have subsided. Read the drug label carefully before taking the medication and ask your medical provider or pharmacist about any side effects or precautions you should take.
It’s important to take your antibiotics at regularly scheduled doses — for example, Amoxil (amoxicillin) may be taken every 8 hours or every 12 hours. This is so the medicine’s effect spreads out evenly over the course of a day. Make sure to ask your medical provider whether to take your medication on an empty stomach or with food to help with medication absorption.
If you miss a dose, take it as soon as you remember. But if it’s closer to your next scheduled dose, generally skipping it and taking your next dose at the regularly scheduled time is recommended. It’s important not to take two doses simultaneously, even to make up for a skipped dose.
- Sharing your antibiotics with others.
- Saving extra antibiotics for later. Instead, take your medication for the length of time your medical provider prescribes.
- Flushing expired antibiotics. Ask your pharmacist for the best way to dispose of old medicines.
- Taking someone else’s antibiotics because you feel sick. This could worsen sickness or cause serious side effects.
Talk to your medical provider if you have questions about your medicine.
Can you drink alcohol while taking antibiotics?
Some antibiotics and alcohol should not be mixed. Mixing alcohol with certain antibiotics, like Flagyl (metronidazole), can worsen side effects like dizziness, drowsiness and stomach upset.
- Flagyl (metronidazole)
- Tindamax (tinidazole)
- Bactrim Septra (sulfamethoxazole-trimethoprim)
- Zyvox (linezolid)
Some antibiotics, when combined with alcohol, can cause more severe reactions such as nausea, vomiting and rapid heart rate. Zyvox (linezolid) may cause dangerous blood pressure spikes when mixed with alcohols like red wine and tap beer.
- Nausea
- Headache
- Dizziness
- Irregular or fast heartbeat
- Flushing
- Abdominal and chest discomfort
- Vomiting
The safety of drinking alcohol while taking specific antibiotics can vary by person and situation. Check with your doctor or pharmacist before drinking alcohol while taking an antibiotic.
Can you eat dairy while taking antibiotics?
Eating dairy products such as butter, cheese, milk and yogurt can interfere with how some antibiotics work. You may have to wait up to three hours after taking an antibiotic to consume dairy products.
Do antibiotics affect birth control?
Some antibiotics may increase the breakdown of estrogen, decreasing the effectiveness of birth control. The antibiotic brand names that could make birth control less effective are Rifadin (rifampin) and Rimactane (rifampin), according to Planned Parenthood and the CDC.

Storing Medicine Properly
In general, antibiotics should be stored in a cool, dry place. However, it’s important to follow the instructions on the drug label and any instructions given by a medical provider or pharmacist regarding your specific antibiotic. Some medicines, like Amoxil (amoxicillin) for example, need to be refrigerated.
Each package of medicine will have an expiration date printed on it, cautioning users against taking antibiotics past this time. According to the FDA, expired antibiotics may fail to properly treat infections and lead to antibiotic resistance.
According to a Harvard article published by Dr. Robert H. Shmerling in 2022, tests on drug stability from the mid-1980s to the early 1990s found that liquid antibiotics showed signs of physical decay after expiration.

Side Effects of Antibiotics
Antibiotics save lives, but nearly one out of five ER visits each year is linked to antibiotic side effects. These side effects are also the most common cause of ER visits for children younger than 18 years of age.
Antibiotics are powerful and not to be misused. The most common side effects are mild. If they worsen or persist, talk to your medical provider.
- Diarrhea
- Nausea and vomiting
- Yeast infection
- Dizziness
- Rash
- Allergic reactions
- Infection caused by C. diff (clostridium difficile)
Allergic Reactions
Before you take antibiotics, tell your medical provider if you have had a history of allergic reactions to penicillin or other antibiotics.
- Swollen face, lips, mouth or tongue
- Difficulty breathing
- Skin rash or hives
- Difficulty swallowing or breathing
- Itching
- Skin peeling or blisters
- Wheezing
- No improvement in the condition
Clostridium Difficile
Antibiotics alter the helpful bacteria in your gut and can lead to an overgrowth of a bacterium called C. diff (clostridium difficile) which can cause severe diarrhea and inflammation of the colon, known as colitis. Tell a medical provider if you develop severe diarrhea, fever, cramping, stomach pain or bloody stool after using antibiotics.
Taking Probiotics with Antibiotics May Help With Side Effects
In the case of diarrhea, abdominal cramping or gas, some research suggests taking a probiotic with your antibiotic may help lessen side effects, according to the Cleveland Clinic. Probiotics include fermented foods like sauerkraut or yogurt.
Probiotics can help with diarrhea caused by C. diff. In fact, one 2022 analysis published in the American Family Physician by Dr. Jennifer Middleton found a 60% reduction in C. diff-associated diarrhea in patients taking probiotics with antibiotics. This benefit may be more significant in patients with a higher risk of developing diarrhea from C. diff. Talk to your doctor to help determine if you are at a higher-than-usual risk.
The most commonly used probiotics for antibiotic-associated diarrhea are L. acidophilus (lactobacillus acidophilus) and S. boulardii (saccharomyces boulardii), which is a kind of yeast. Before taking probiotics, ask your medical provider or pharmacist if they are safe for you.

Antibiotic Resistance
Antibiotic resistance occurs when bacteria develop ways to protect themselves against antibiotics.
“If you keep using the same antibiotics routinely, the bugs mutate, and they can live through antibiotic treatment,” immunologist and thoracic surgeon Dr. Hooman Noorchashm told Drugwatch.
In July 2024, the CDC reported that hospitals saw a 20% increase in infections that don’t respond to antibiotics during the COVID-19 pandemic. The issue peaked in 2021 and remained high in 2022.
Antibiotic resistance is one of the most urgent threats to public health. It affects the health of people, animals and the environment.
According to the CDC, antibiotic-resistant bacteria cause more than 2.8 million infections annually, and more than 35,000 people die each year because of them.
- Penicillin, released in 1941
- Staphylococcus aureus (staph infection), Streptococcus pneumoniae (pneumonia, ear infections, sinus infections and meningitis), Neisseria gonorrhoeae (gonorrhea)
- Vancomycin, released in 1958
- Enterococcus faecium (endocarditis, prostatitis, urinary tract infections, intra-abdominal infection, wound infection and cellulitis), Staphylococcus aureus (staph infection)
- Ciprofloxacin, released in 1987
- Neisseria gonorrhoeae (gonorrhea)
- Ceftazidime-avibactam, released in 2015
- Ceftazidime-avibactam-resistant KPC-producing Klebsiella pneumoniae (pneumonia, wound or surgical site infections, bloodstream infections and meningitis)
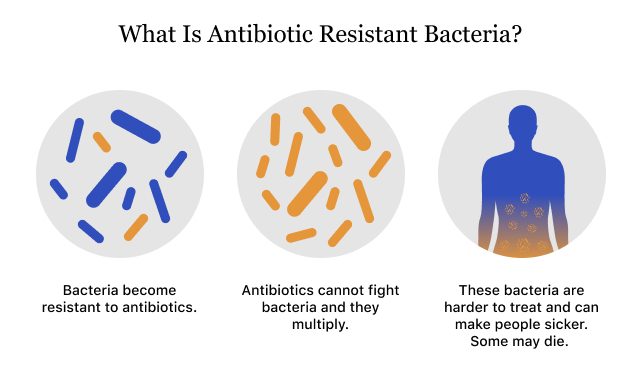
Antibiotic resistance can occur anytime antibiotics are used. That’s why it’s important to use antibiotics only when necessary. If your doctor determines that you do not have an infection that needs antibiotics, consider other solutions provided by your medical team. The CDC estimates that about 47 million antibiotics are prescribed for infections, like the cold and flu, and that these drugs do not need to be taken.
Another way you can help prevent the threat of antibiotic resistance is to take antibiotics as directed for the full length of treatment to kill all organisms. Dispose of expired antibiotics and ensure you are the sole recipient of your prescription.

Takeaways for Using Antibiotics Safely
Dr. Hooman Noorchashm has prescribed antibiotics to his patients for years. He recommends these quick, basic tips for taking antibiotics safely.
- Get a Specific Diagnosis
- “You want to make sure that there’s a specific bug that you are afflicted by and have a diagnosis for, like strep throat for example,” Noorchasm said. “You don’t want to take antibiotics just because you feel sick.”
- Antibiotics Are Not for Preventing Sickness
- “You don’t want to take antibiotics prophylactically (to prevent illness) unless your medical provider has given you a clear indication,” said Noorchashm. “For example, some patients with heart valves who are going to have a dental procedure have to take antibiotics to prevent infections.”
- Communicate Allergies
- “Tell your medical provider about any known allergies to penicillin (or other antibiotics) to make sure they don’t give you that class of antibiotics,” said Noorchashm.
- Ask About Side Effects
- “All of these drugs at a certain rate will cause adverse events, anywhere from colitis from C. diff to nerve damage and hearing loss,” Noorchashm said. “This is why you don’t want to use them unless you are treating a real bacterial infection.”
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.

