Veterans Health Guide
Military veterans experience a range of service-related health conditions, including hearing damage, traumatic brain injury (TBI), post-traumatic stress disorder (PTSD) and toxic exposure to asbestos and burn pits. The U.S. Department of Veterans Affairs (VA) offers health benefits and disability compensation to veterans, and a number of resources and support programs exist to help veterans and their families live healthier lives.

Military veterans face health issues resulting from physical and mental stress related to combat. These stressors can occur during wartime and peacetime or simply during routine training exercises, and they differ significantly from those faced by civilians.
“The military is in the business of war fighting. It’s a dangerous occupation by its very nature, so it comes with a lot of occupational hazards,” Veterans of Foreign Wars (VFW) National Veterans Service Ryan Gallucci told Drugwatch.
When veterans return to civilian life, it can be a shock. Maintaining mental and physical health can fall by the wayside.
“We call it the ‘warrior ethos,’” Gallucci, an Iraq war Army veteran, said. “When you are in the military, if you have a problem, it almost is a joke that you drink water, change your socks and stay motivated. If it is really bad, pop a couple of Motrin.”
Fortunately, resources for treating service-related conditions, acclimating to civilian life and staying healthy are available to veterans. Veterans should use these earned benefits.
The U.S. Department of VA provides many of these resources, but other nonprofit organizations, such as VFW, work with the VA and help veterans access benefits and support groups.

Hearing Loss and Tinnitus
Hearing problems such as tinnitus — ringing in the ears — and hearing loss are the most prevalent health conditions treated at VA medical centers, according to Hearing Health Foundation. Veterans are 30% more likely than nonveterans to have a severe hearing impairment, according to the Centers for Disease Control and Prevention (CDC).
Congress authorized the creation of The Hearing Center of Excellence to study, prevent, and treat veterans with hearing loss and auditory injuries. Veterans and their families can find audiologists and information about resources such as assistive technology on the website.
You May Have Hearing Damage If You:
- Develop ringing or buzzing in your ears
- Feel “fullness” in your ears after leaving noisy places or events, such as a concert
- Find it difficult to hear someone talking from three feet away
- Have problems understanding what people are saying
Tinnitus and hearing loss are the top reasons for veterans to seek disability benefits. Veterans with service-related tinnitus and hearing loss may apply for VA disability benefits or hearing aids, according to the Hearing Center of Excellence.
“Whether it’s one ear or both ears, tinnitus has a maximum benefit rate of 10%,” Gallucci said. “That’s as high as it can go. That’s as high as it will ever go. That’s what VA’s rating schedule and regulations prescribe.”
Hearing Loss Causes and Treatment
Loud noises from explosions, weapons and military vehicles and machinery are unavoidable for most active service men and service women.
According to the CDC, the prevalence of hearing impairment is greater for veterans who served after September 2001, particularly veterans who served in Operation Enduring Freedom and Operation Iraqi Freedom, compared with other veterans. These operations exposed veterans to roadside bombs and other improvised explosive devices (IEDs).
The sound wave from a blast can damage the eardrum (tympanic membrane) and middle ear. These injuries are common but may heal on their own or be treated with surgery. Hearing aids might also help.
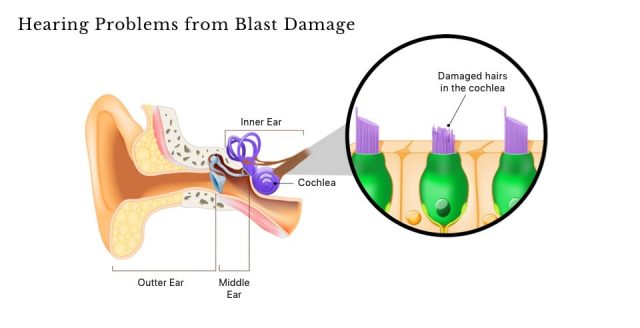
The most devastating injuries occur when blast waves damage the cochlea — a snail-shell-shaped organ deep in the inner ear. Damage to small hairs inside the cochlea can cause permanent, disabling hearing loss or tinnitus.
Another possible cause of hearing problems is exposure to jet propulsion fuel in combination with noise.
In a 2014 study published in the Journal of Toxicology and Environmental Health, authors found that veterans who are exposed to jet fuel may pass hearing tests but not understand what they are hearing because of a brain dysfunction.
3M Combat Arms Earplugs
Protective gear, such as earmuffs and earplugs, helps soldiers avoid service-related hearing disorders. In fact, many soldiers between 2003 and 2015 received 3M’s Dual-Ended Combat Arms earplugs during their service.
But in July 2018, 3M paid $9.1 million to the U.S. Department of Justice to settle allegations that it had sold faulty Combat Arms Earplugs to the military. In court documents, whistleblowers claimed that 3M had exposed millions of soldiers to the risk or hearing loss and tinnitus.
The whistleblower lawsuit led many veterans to file lawsuits against 3M for hearing damage. Lawsuits against 3M don’t affect disability benefits.

Vision Loss
Veterans may suffer vision problems as a result of age or service-related injuries. Major causes of age-related vision loss include diabetic retinopathy, macular degeneration, cataracts, stroke and glaucoma.
Blast-related brain injuries in veterans of operations in Iraq and Afghanistan may cause blurred vision, sensitivity to light, reading impairments and double vision, according to the VA’s research on vision loss.
Approximately 130,000 American veterans are legally blind, and more than one million veterans have vision problems that make it difficult to do daily tasks, according to the VA’s Office of Blind Rehabilitation Services.
“Here I was, living in the sighted world for 26 years, and then I woke up one day and I was totally blind. Now I have to rewire myself to use my hands as my eyes.”
The cost of service-related vision problems between 2000 and 2010 exceeded $25 billion, according to a 2017 study published in Clinical & Experimental Ophthalmology.
Former Staff Sargent Jason Pepper recounted his experience with vision loss from an IED blast in an article published by the American Academy of Ophthalmology.
“Here I was, living in the sighted world for 26 years, and then I woke up one day and I was totally blind. Now I have to rewire myself to use my hands as my eyes,” Pepper said.
After several surgeries and prosthesis fittings, Pepper has learned to live with his disabilities and has even gone skiing, proving the power of proper care and a resilient spirit.
VA Services for Blind and Vision-Impaired Veterans
Congress authorized the Secretary of Defense to establish the Vision Center of Excellence in 2008. The center’s goal is to improve vision health and enhance quality of life for veterans and active service members.

The VA operates 13 Blind Rehabilitation Centers across the country, 22 intermediate and advanced low-vision clinics and 23 advanced ambulatory low-vision clinics.
These facilities help veterans adjust to blindness and low vision. Rehabilitation centers help veterans with communication skills, social activities, manual skills, orientation and mobility and accomplishing daily tasks.
Veterans may file for disability for visual impairments such as blurry vision, loss of sight, double vision, loss of light perception and loss of peripheral vision. In order to file for disability benefits, a licensed ophthalmologist or optometrist must examine them.
Gallucci notes that veterans can’t claim certain vision problems.
“If you are near-sighted, for example, and you didn’t wear glasses before you went in the military, but you wear glasses now,” he said. “That’s considered a congenital condition. You are not able to have it service connected.”

Mental Health and PTSD
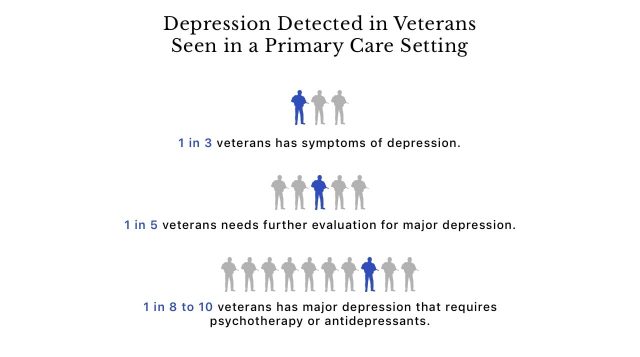
In addition to physical health issues, a large number of veterans may also face mental health disorders such as depression and anxiety caused by traumatic brain injuries. Service members may also experience military sexual trauma (MST) and post-traumatic stress disorder (PTSD). These are often referred to as “invisible injuries.”
“They’ve always been there,” Gallucci said. “In World War I they called PTSD shell shock. It wasn’t a clinical diagnosis until the 1980s. But now that it is a clinical diagnosis and we understand a little bit more about it, it’s become more common.”
In extreme cases, these conditions may lead to suicide. The 2019 National Veteran Suicide Prevention Annual Report revealed that in 2017 there were 6,139 veteran suicide deaths, an increase of 129 suicide deaths in 2016.
The VA Center of Excellence for Stress and Mental Health provides veterans with resources for stressful life events and challenges after leaving the military. Caregivers and family members can also get information.
Military Sexual Trauma (MST)
The VA defines military sexual trauma, or MST, as “psychological trauma, which in the judgment of a VA mental health professional, resulted from a physical assault of a sexual nature, battery of a sexual nature, or sexual harassment which occurred while the Veteran was serving on active duty, active duty for training, or inactive duty training.”
Examples of MST include a service member enduring sexual activity against his or her will, including through force, coercion or when incapable of consent; being touched in uncomfortable sexual ways; being exposed to repeated comments about his or her body or sexual activities and unwanted sexual advances.
In 2015, the data from the VA national screening program revealed that about 1 in 4 women and 1 in 100 men experienced MST during provider screenings.
Manifestations of MST
- Alcohol or drug misuse
- Concentration, attention or memory difficulties
- Difficulty in relationships, abusive relationships, difficulty trusting others
- Emotional numbness (trouble experiencing happiness or love)
- Feeling edgy, jumpy or vulnerable
- Avoiding reminders of the experience
- Physical health problems (weight gain, eating disorders, chronic pain, sexual dysfunction)
- Sleep disorders (nightmares, trouble falling or staying asleep)
- Heightened emotions (depression, intense emotional reactions, anger and irritability)
While more women than men experience MST, substantial numbers of both genders experience MST, according to the VA data .
The VA stresses that MST is an experience — not a condition. Military sexual trauma can affect physical and mental health for many years. Each local VA center has an MST coordinator who can assist veterans.
The Five Signs of Emotional Suffering
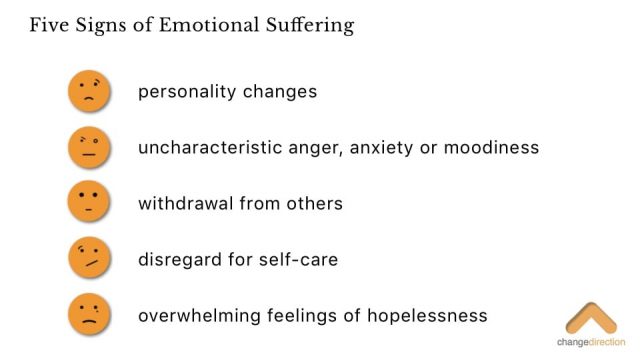
The Five Signs of Emotional Suffering can help you recognize that you or a fellow veteran may be suffering from PTSD, depression or another mental disorder. These signs include personality changes, uncharacteristic anger, anxiety or moodiness, withdrawal from others, disregard for self-care, and overwhelming feelings of hopelessness.
Post Traumatic Stress Disorder (PTSD)
Post-traumatic stress disorder, or PTSD, affects people who have been exposed to horrible or life-threatening situations. It can happen to anyone, but it occurs often in veterans because of the extreme nature of combat situations.
Rates of PTSD are higher for veterans of specific wars, according to the VA’s National Center for PTSD. Veterans who have experienced MST can also have PTSD.
Number of Veterans with PTSD by Service Area
- 11% to 20% of veterans who served in Operation Iraqi Freedom and Operation Enduring Freedom are diagnosed with PTSD every year.
- 12% of veterans who served in the Gulf War are diagnosed with PTSD every year.
- An estimated 30% of Vietnam War veterans have had PTSD in their lifetime.
Researchers have found that PTSD is linked to chronic body pain, high blood pressure, high cholesterol, obesity and cardiovascular disease. Treating PTSD may improve overall health.
Some studies also link PTSD to gastrointestinal problems such as gastroesophageal reflux disorder (GERD), acid reflux and irritable bowel syndrome (IBS). Veterans who experience these GI problems as a result of PTSD are typically prescribed drugs such as proton pump inhibitors (PPIs) and H2 blockers by the VA. Some veterans who were diagnosed with cancer after taking the antacid Zantac for their GI problems have filed lawsuits against the drug’s manufacturers.
For example, a 2019 study published in JAMA Psychiatry found that decreasing PTSD symptoms could lower the risk of Type 2 diabetes in veterans.
VA disability benefits cover PTSD. Veterans must have a current diagnosis of PTSD, a statement about the stressful event that triggered PTSD and a medical opinion from a VA-approved psychiatrist or psychologist affirming the association between PTSD and the veteran’s service.
Gallucci said two of the best ways to manage PTSD are to stay active and seek peer support groups.
Help for PTSD or Mental Distress
Post-traumatic stress disorder and other mental disorders stemming from trauma are serious conditions that can have life-threatening consequences. Veterans who have given so much for their country should never be alone in times of need. Free, confidential 24/7 crisis counseling is just a text or phone call away.
- Crisis Text Line
- Text SIGNS to 741741
Not veteran specific. - Suicide Prevention Lifeline
- 1-800-273-TALK (8255)
TTY: 1-800-799-4889
Not veteran specific. - Vets4Warriors
- 1-855-838-8255
DSN: 312-560-1110
Veteran specific.

Substance Use Disorders
Many veterans suffer from substance use disorders (SUDs). Veterans with multiple deployments, combat exposure and injuries are at the greatest risk.
Heavy drinking and cigarette smoking are the most prevalent types of SUDs. But opioid misuse is on the rise.
About 1 in 10 returning veterans of the wars in Iraq and Afghanistan seen by VA doctors have a problem with alcohol or other drugs. According to the VA, veterans with PTSD have an increased risk for SUDs.
VA medical centers across the country offer help for veterans. Groups such as Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) can also provide support.
Treatment for SUDs includes behavioral therapies, such as motivational interviewing and medication-assisted treatment. Behavioral therapy can help a veteran identify and modify thoughts that lead to substance misuse.
A 2017 randomized, controlled trial of 242 Army personnel who met the DSM-IV criteria for alcohol use disorder, which was published in the Journal of Consulting and Clinical Psychology, revealed that just one session of motivational interviewing plus feedback resulted in fewer drinks per week and lower rates of alcohol dependence in participants.
In addition to behavioral and talk therapy, some medications may reduce withdrawal symptoms and cravings.
Medications for alcohol use disorders include naltrexone, acamprosate and disulfiram. Drugs used for opioid treatment include methadone, buprenorphine, naltrexone and extended-release injectable naltrexone.
Private addiction rehabilitation centers may also have programs that provide support to veterans.
- U.S. Department of Veterans Affairs
- The VA offers various programs for veterans seeking treatment for addiction. To find the program that’s right for you, speak with your VA health care provider or call 1-800-827-1000.
- SAMHSA’s National Helpline
- The Substance Abuse and Mental Health Services Administration (SAMHSA) offers a wealth of resources for people with mental health or substance use disorders. You will get access to local treatment centers, support groups and community organizations by calling 1-800-662-HELP (4357), 24 hours a day and free of charge.

Traumatic Brain Injury
Traumatic brain injury, or TBI, can affect veterans subjected to bumps, blows or jolts to the head during service. Most cases of TBI in the military occurred after blast injuries from IEDs. Many veterans of the Iraq and Afghanistan wars who were exposed to IEDs have experienced TBI.
The VA estimates that 22% of all combat casualties from the wars in the Middle East were brain injuries.
Symptoms of TBI vary by the severity of the injury, but they usually involve headaches, dizziness, problems walking, fatigue, irritability, changes in personality and memory and attention problems.
Health providers diagnose TBI and its severity by using CT scans and collecting information about the injury, including loss of consciousness and memory. Treatment for TBI involves therapy to help with speech, cognition and physical impairment. Providers may also prescribe medication for anxiety or headaches.
Veterans with TBI are eligible for a disability rating of up to 100%, depending on the severity of their condition.

Environmental Hazards and Chemical Exposures
Military service exposes soldiers to high-stress situations in combat, but it can also expose them to hazardous chemicals and substances. These can lead to potentially fatal illnesses and diseases that affect quality of life. For example, many veterans exposed to asbestos used for fireproofing later developed an aggressive cancer called mesothelioma.
Veterans of the Gulf War who served in Southwest Asia were exposed to oil-well fires, pesticides and vaccinations that may have led to medically unexplained illnesses, such as severe fatigue, fibromyalgia and gastrointestinal disorders. The military calls this “Gulf War illness” or “chronic multisymptom illness.”
Military Exposure Categories
- Chemicals (contaminated water, Agent Orange, pesticides, depleted uranium, industrial solvents)
- Radiation (nuclear weapons testing, X-rays)
- Air pollutants (burn pits, oil-well fire, sand and dust, combustion-waste disposal)
- Occupational hazards (asbestos, lead, polychlorinated biphenyl used as coolant, fuels)
Veterans who can prove that the illness or disease resulted from exposure to a harmful substance during service may qualify for disability compensation.
Get help and learn more on the VA’s military exposures webpage.
Toxic Chemicals at Camp Lejeune
Veterans and service members may also be exposed to toxic chemicals in contaminated water at military bases. One of these is Marine Corps Base Camp Lejeune in North Carolina.
“So, when I talk about toxic exposure, we’re not just talking about Agent Orange. There was water contamination on Camp Lejeune in the 1980s that the Department of Veterans Affairs now acknowledges,” said Gallucci.
The government discovered that toxic chemicals, including cancer-causing chemicals such as benzene and trichloroethylene, also known as TCE, had contaminated the water at Camp Lejeune. People who lived and worked at the base from 1953 to 1987 could have been exposed to these chemicals and suffered serious health problems.
The VA provides disability benefits and health care reimbursement for out-of-pocket expenses related to Camp Lejeune health problems. In August 2022, President Joe Biden signed the PACT Act of 2022 into law, which includes the Camp Lejeune Justice Act. This law removes restrictions that prevented Camp Lejeune veterans and others from suing the government for compensation for injuries.

VA Health Benefits and Disability Claims
Veterans are eligible for VA health care benefits if they served in any branch of the military and didn’t receive a dishonorable discharge. Personnel who enlisted after Sept. 7, 1980, or entered active duty after Oct. 16, 1981, must have served 24 continuous months of active duty to qualify.
Veterans can apply on the VA application page, in person at a local VA medical center or by calling 1-877-222-8387.
Have your most recent tax return, your social security number, your dependents’ social security numbers, and account numbers for your current health insurance. Make sure to fill out an Application for Health Benefits (VA Form 10-10EZ). It takes less than a week to find out if you qualify.
What If I Can’t Get to a VA Medical Center?
The VA Mission Act, signed into law in 2019, makes VA health care more accessible to veterans in rural areas or veterans who have difficulty getting to a VA center or clinic by allowing veterans to see civilian health providers within the VA network who may be closer to home.
The VA has also been making advances in telehealth. Veterans can connect with VA providers via telephone or internet.
VA health care now includes urgent care access through a network of walk-in clinics and urgent care facilities nationwide.
In addition, the VFW partnered with the VA to establish Project Atlas, an initiative to install telehealth facilities in local VFW posts.
“Basically where VA doesn’t have a presence, there are certain things they can do,” Gallucci said. “There are things you can do with telehealth blood pressure monitoring, heart rate monitoring, even some minor clinical things that the average veteran could handle on the spot remotely, or to determine if there is a medical emergency.”
Disability Claims
The VA offers disability benefits or compensation to veterans whose illnesses or injuries were caused or made worse by active military service. Applicants must have served on active duty, active duty for training or inactive duty training and have received a disability rating.
Gallucci, who guides veterans through the process of filing disability claims, has advice for veterans.
- Don’t do it alone, but don’t pay someone to file your claim.
- Experienced Veterans Service Officers can help you file your claim for free. According to Gallucci, some people might want to charge you to file your claim. It’s illegal to charge.
- While you need medical records, you might not need them to file.
- The VA can acquire any military or federal records for you, and they have a duty to do so. You can also sign a release for the VA to get records from civilian health care providers, but they don’t have an obligation to do so. It may be easier to get these records yourself.
- Get a lay or buddy statement.
- Supporting statements that explain how the illness or injury occurred or got worse can help your claim. These statements, which can come from family, friends, law enforcement, military personnel you served with or clergy members, may also illustrate how symptoms affect your daily life or relationships.
- Remember the VA process is nonadversarial.
- The VA is trying to verify that a condition is related to your military service and that it impairs your life, Gallucci said. In the process, they may triple check your claim and require you to see a VA compensation examiner. This examiner will determine your occupational and social impairment.
The VA assigns veterans a disability rating based on doctors’ reports, any VA claim exams and other information from federal agencies.
After the applicant submits a claim, the VA reviews the documents, gathers and reviews evidence and documents to support its decision. The claim’s status is then “pending a decision.” Once the decision is made, the VA mails all the documents to the applicant. These documents will include the details of the decision or award.
The amount of compensation may be affected by military retirement pay, disability severance pay or separation pay and whether you were incarcerated for more than 60 days or convicted of a felony.
For more details, visit the VA’s disability benefits page.

Service Officers Help Veterans with Claims
Navigating the world of VA benefits and disability claims can be complicated, but accredited Veterans Service Officers can help.
Veterans Service Officers can help veterans and their families understand their benefits and file for disability claims. Veterans are entitled to this free service.
The VFW is one of the oldest and largest nonprofit organizations dedicated to training service officers accredited by the VA to assist veterans with filing for benefits.
“There are some — what I would call — ‘bad actors’ out there that would charge consulting fees to help you file your VA claim. You don't need to do that. In fact, it is illegal.”
“VA does make resources available. You can go online, and you can do it yourself. But the IRS also does that for taxes. Many times it’s in your best interest to work with a tax accountant who’s equipped to handle that. A Veterans Service Officer who is accredited through VA, like the VFW’s service officers, are equipped to do that,” Gallucci said.
Each state provides Veterans Service Officers. But several organizations, such as the VFW, can also provide help. Additionally, some attorneys can help veterans file their claims free of charge.
Organizations that Provide Veterans Service Officers
- Veterans of Foreign Wars
- AMVETS
- Vietnam Veterans of America
- Disabled American Veterans
- Paralyzed Veterans of America
- American Legion
- Military Order of the Purple Heart

General Health Tips
Everyone benefits from good nutrition and exercise, even veterans. The VA offers several programs for overall wellness, too. Your local VA center or clinic can tell you about the programs they offer.
Use Your Benefits
According to Gallucci, the VFW’s survey data show that a large margin of veterans would recommend VA care to their fellow veterans. He also said veterans who use VA health care are more likely than those who don’t to be satisfied with the VA.
“Don’t be afraid to use the VA benefits you are entitled to,” Gallucci said. “That’s what they are there for. These benefits are there to help in what can be an often-difficult transition from military to civilian life.”
Another benefit to seeking help from the VA is that VA providers are often better equipped than civilian doctors to treat service-related health problems.
Eat Right, Exercise
The military stresses eating right and getting exercise, and many service members learn the basics in active duty. But when veterans leave the military, these activities can be difficult.
“For those who suffer from conditions like post-traumatic stress disorder, it’s well documented that regular exercise helps — especially if you exercise with other people,” Gallucci said.
Many gyms and group classes serve athletes who need adaptive movement. Many VFW posts also offer group fitness classes.
“You find severely wounded veterans who compete in marathons, CrossFit, yoga, different types of activities. We have a VFW post in Colorado, VFW Post 1, that hosts regular yoga at their post. My post, VFW Post 3150 in Arlington, VA, does it from time to time as well,” said Gallucci.
Find a Tribe, Get Involved
Isolation is detrimental to veterans. If they are dealing with service-related injuries or disabilities, they may feel even more alone.
“So many times getting out with another group of veterans and finding a tribe or something like that is incredibly therapeutic,” Gallucci said. “One of our foundational values is peer-to-peer support and finding a network of like-minded veterans. It helps with so many other things.”
While in-person support is the gold standard, connecting through support groups online works, too.
Look for Facebook groups or organizations, such as Vets4Warriors and Patients Like Me, that connect veterans and others with similar health issues.
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.


