Valsartan: Recall, Contamination Risks and Side Effects
Tests show valsartan was contaminated with NDMA and NDEA, which are known carcinogens. Manufacturers recalled the medication, but some people already suffered injuries and are now pursuing legal claims to hold the drug makers responsible for their dangerous products.
Our content is developed and backed by respected legal, medical and scientific experts. More than 30 contributors, including product liability attorneys and board-certified physicians, have reviewed our website to ensure it’s medically sound and legally accurate.
legal help when you need it most.
Drugwatch has provided people injured by harmful drugs and devices with reliable answers and experienced legal help since 2009. Brought to you by Wilson & Peterson LLP, we've pursued justice for more than 20,000 families and secured $324 million in settlements and verdicts against negligent manufacturers.
More than 30 contributors, including mass tort attorneys and board-certified doctors, have reviewed our website and added their unique perspectives to ensure you get the most updated and highest quality information.
Drugwatch.com is AACI-certified as a trusted medical content website and is produced by lawyers, a patient advocate and award-winning journalists whose affiliations include the American Bar Association and the American Medical Writers Association.
About Drugwatch.com
- 15+ Years of Advocacy
- $324 Million Recovered for Clients
- 20,000 Families Helped
- A+ BBB Rating
- 4.9 Stars from Google Reviews
Testimonials
I found Drugwatch to be very helpful with finding the right lawyers. We had the opportunity to share our story as well, so that more people can be aware of NEC. We are forever grateful for them.
- Medically reviewed by Mireille Hobeika, Pharm.D.
- Last update: August 1, 2025
- Est. Read Time: 4 min read
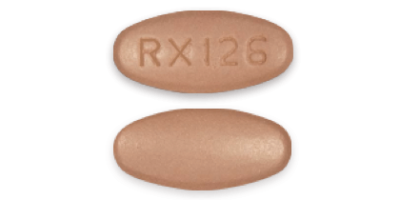
Valsartan is a heart medication that primarily treats high blood pressure. Manufacturers recalled many pharmaceuticals containing valsartan between 2018 and 2021 due to dangerous chemical impurities.
Medications containing valsartan may have links to an increased risk of various types of cancer due to exposure to carcinogenic compounds called nitrosamines. Patients who used the medication before the valsartan recalls are now pursuing litigation to hold manufacturers liable for their injuries.
- Valsartan was contaminated with the carcinogens NDMA and NDEA
- Numerous manufacturers faced recalls due to contaminated active pharmaceutical ingredients (API)
- Patients who used valsartan may face an increased cancer risk
What Is Valsartan?
Valsartan is a prescription medication used to treat high blood pressure and heart failure. Manufacturers have sold valsartan under the brand names Diovan and Prexxartan.
Valsartan is part of a class of drugs called angiotensin II receptor antagonists (ARBs), which block natural processes that cause blood vessels to tighten. By blocking these processes, valsartan allows the heart to pump more effectively and for blood to flow more easily.
Why Did Manufacturers Recall Valsartan?
Drug makers recalled valsartan because the U.S. Food and Drug Administration (FDA) determined that medications like valsartan made with active pharmaceutical ingredients (APIs) from labs in China and India contained dangerous impurities.
A number of FDA recalls have occurred due to problems with valsartan, including the following:
- July 13, 2018:
- Major Pharmaceuticals voluntarily recalled all lots of valsartan supplied by Teva Pharmaceuticals. The recall occurred after the discovery of trace amounts of an impurity called N-Nitrosodimethylamine (NDMA). The International Agency for Research on Cancer (IARC) classifies NDMA as being “probably carcinogenic to humans.”
- July 16, 2018:
- Prinston Pharmaceutical Inc. voluntarily recalled valsartan and valsartan-hydrochlorothiazide tablets due to potential NDMA contamination.
- July 17, 2018:
- Teva Pharmaceuticals recalled valsartan and valsartan-hydrochlorothiazide tablets sold under the Actavis label as a result of trace amounts of NDMA.
- August 7, 2018:
- Camber Pharmaceuticals recalled all unexpired lots of valsartan after testing confirmed the presence of NDMA.
- August 17, 2018:
- Torrent Pharmaceuticals recalled all lots of valsartan and valsartan-containing medications due to NDMA impurities.
- September 13, 2018:
- Torrent Pharmaceuticals expanded its recall to include three lots of valsartan drugs, which the FDA found were contaminated with a second potentially carcinogenic impurity, N-Nitrosodiethylamine (NDEA).
From 2019 through 2021, the FDA tracked recalls for 1,246 lots of valsartan medications. The FDA maintains an updated list of recalled valsartan products, which the agency last modified in late 2021, to alert patients if their medications were part of the recall.
Recalls were not isolated to the United States. In fact, the FDA’s actions only came after 22 other countries issued recalls of 2,300 batches of contaminated valsartan. The recalls were so widespread because global suppliers introduced the impurities before sending APIs to many other companies across different countries.
What Is NDMA and Why Is It Dangerous?
NDMA is a chemical that forms during natural and industrial processes. The human body creates low levels of NDMA, and it’s also unintentionally produced by chemical reactions in labs. For instance, the wastewater disinfection process may form NDMA as a byproduct.
In addition to the IARC, the U.S. Department of Health and Human Services (HHS) and the Environmental Protection Agency (EPA) classify NDMA as a “probable” or “reasonably anticipated” carcinogen.
In 2018, the European Medicines Agency announced it had detected an average NDMA level of 60 parts per million in valsartan manufactured by certain global suppliers.
NDMA at this level could result in one additional patient developing cancer out of every 5,000 patients taking valsartan in the highest allowable dose (320 mg) each day for seven years.
Before 2018, NDMA contamination was not an expected or known valsartan side effect, so patients who used it did not know about the potential risk of exposure to this potentially carcinogenic substance.
Not all valsartan products were contaminated — only those manufactured by affected labs, including Zhejiang Huahai Pharmaceutical Co. Ltd. in China and Mylan Pharmaceuticals in India.
Valsartan Side Effects
Even when valsartan isn’t tainted with NDMA, it can cause several different types of side effects. Drug makers, including valsartan manufacturers, must tell patients and health care providers about the side effects of the medications they produce.
- Blurry vision
- Cough
- Diarrhea
- Dizziness
- Headaches
- Increased potassium levels
- Increased risk of viral infection
- Joint or muscle pain
- Low blood pressure
- Nausea
- Vertigo
- Vomiting
- Kidney issues
- Low blood cell count
- Severely elevated potassium levels
- Very low blood pressure
Valsartan also carries a black box warning — the FDA’s most serious warning —alerting patients of serious potential risks to unborn babies.
Valsartan Contamination and Cancer Risk
Valsartan recalls were necessary due to the links between NDMA contamination and various types of cancer. Specifically:
- A study published in the Journal of the American Heart Association found a link between exposure to NDMA in valsartan and an increased risk of liver cancer and melanoma.
- A study published by Deutsches Ärzteblatt International found a link between taking NDMA-contaminated valsartan and hepatic (liver) cancer.
- A Danish study published in the medical journal BMJ found that NDMA exposure increased the risk of colorectal and uterine cancers.
How To Know if You Took Recalled Valsartan
The best way to determine if you took recalled valsartan is to check the FDA’s database of recalled lots of valsartan medications. You will need to know your lot number, which you can find:
- By checking the bottle or vial, if you have any remaining pill bottles at home. The lot number is typically by the barcode or under the dosing instructions.
- By contacting your pharmacy or doctor for information, if you no longer have the bottles.
The affected medications were primarily sold between 2014 and 2018, so it may be unlikely that you still have the medication bottles. However, your medical records and pharmacy records should have the information you need.
What To Do if the Valsartan Recall Affects You
If you took recalled valsartan, there are a few steps you can take to protect your health going forward:
- Discuss screening or health monitoring with your doctor to watch for early signs of cancer due to the valsartan cancer risk.
- Report any concerning symptoms to your doctor immediately so you can undergo proper testing.
- Save your prescription records, pill bottles and other documentation.
You may also wish to file a valsartan lawsuit to hold the drug manufacturers accountable. You can speak with an attorney to explore your options, including joining a multidistrict litigation (MDL) with other valsartan users in a consolidated case.
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.