
Depression
Depression, also known as clinical depression or major depressive disorder, is a mood disorder that causes intense sadness lasting at least two weeks or more. It can interfere with a person’s ability to function and perform daily tasks. Treatment options include psychotherapy, medication and brain stimulation therapy.
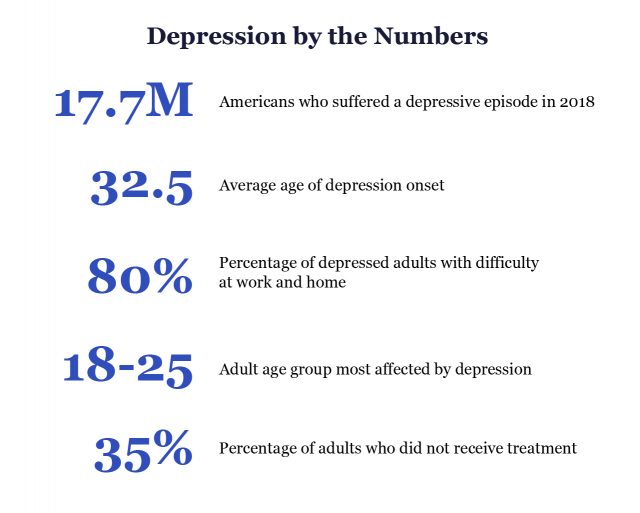
Depression is a common disorder. About 17.7 million American adults had at least one major depressive episode in 2018, according to the Substance Abuse and Mental Health Services Administration, or SAMHSA.
It affects 264 million people and is a leading cause of disability worldwide, according to the World Health Organization.
Clinical depression is more than just being sad about the death of a loved one, being in a bad mood or being upset about a lost relationship. If left untreated it can cause people to lose sleep, stop eating or lose their jobs.
For people with chronic diseases, such as diabetes, depression can affect their ability to care for themselves. For example, people with diabetes are up to 3 times more likely to have depression than people without diabetes, according to the Centers for Disease Control and Prevention.
Everyone can suffer from depression, but different groups such as young people, women and LGBTQ+ individuals may have a higher risk for depression.
Fortunately, there are several treatment options and resources available. With these treatments and a good social support system, people diagnosed with depression can improve their health and successfully control their symptoms.
What Are the Symptoms?
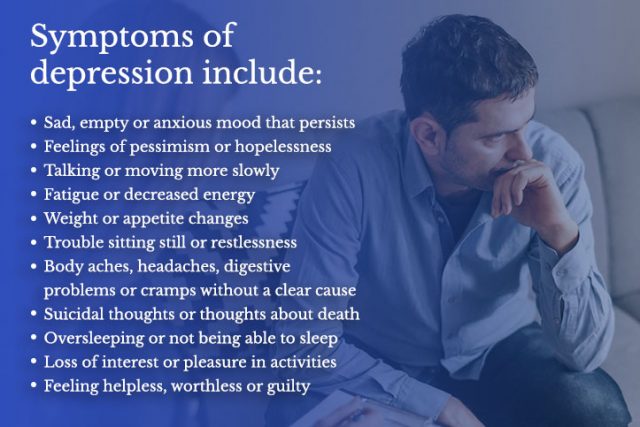
Each person experiences different symptoms of depression. The disorder causes a mix of mental and physical symptoms. The length of time these symptoms last varies depending on the person. The type of depression a person has can also affect the symptoms and severity.
Clinical depression symptoms can affect people at any age, but the average age of onset is 32 and a half years old, according to the Anxiety and Depression Association of America.
Other medical conditions may have similar symptoms to depression. These include thyroid problems, vitamin deficiencies and brain tumors. It’s important to talk to a health care provider to rule out these conditions.
If a person suffers from several of these symptoms nearly every day for at least two weeks, they may have depression and should seek help from a health care provider.
What Are the Major Types?
Major depressive disorder is the primary type of depression, but there are a few subtypes, according to the National Institutes of Mental Health.
Each type of depression may manifest symptoms differently. The distinguishing factor between these types is timing and consistency of symptoms. The type of depression someone has affects the type of treatment a health care provider may recommend.
The most common include persistent depressive disorder, postpartum depression, psychotic depression, seasonal affective disorder and bipolar disorder.
Persistent Depressive Disorder (Dysthymia)
Persistent depressive disorder manifests the same symptoms of major depressive disorder, but the symptoms last for least two years or more.
People with major depressive disorder may cycle in and out of depression, but people with dysthymia suffer with persistent symptoms for years. Dysthymia episodes may be less severe, but they are longer lasting.
Persistent depressive disorder starting before age 21 is considered early onset. After 21, it is late onset.
Postpartum Depression
Many women suffer mild anxiety and depression within two weeks of giving birth. But women who have postpartum depression experience longer-lasting symptoms of major depressive disorder, both during and up to a year after pregnancy.
This makes it difficult for a mother to take care of her baby. In addition to the symptoms of clinical depression, postpartum can make it difficult for mothers to bond with their babies and make them think about hurting themselves and their babies.
The condition occurs in about 15 percent of births, according to the National Institute for Mental Health. It usually affects mothers between a week and month after delivery, but can begin anytime shortly before or after childbirth.
Psychotic Depression
People with psychotic depression experience symptoms of major depressive disorder but also have symptoms of psychosis such as delusions or hallucinations. Psychotic depression occurs in about 14 to 20 percent of people with major depressive disorder.
These people may have delusions such as believing they are poor, are guilty or have a serious illness like cancer. Hallucinations may manifest as voices telling them they are worthless or that they should harm themselves.
Psychotic depression is serious and requires immediate medical treatment because the risk for suicide is higher in people with this condition, according to the National Library of Medicine.
Approximately 20 percent of people with psychotic depression attempt suicide during an episode, according to Psychiatric Times.
Seasonal Affective Disorder (SAD)
Seasonal affective disorder manifests as depression that occurs when there is less sunlight in the winter months. Symptoms typically go away in spring and summer. Between 5 and 10 percent of Americans experience SAD, according to Time magazine.
To be diagnosed with SAD, people have to have depression that coincides with the seasons for at least two years. In addition to the typical symptoms of depression, people with SAD may suffer from weight gain, overeating and cravings for carbohydrates during the winter months.
Bipolar Disorder
Bipolar disorder was once called manic-depressive illness or manic depression. People with bipolar disorder can experience extreme highs and lows in mood. This disorder is different from depression, but people with this condition can experience lows that have symptoms of major depression.
About 2.8 percent of U.S. adults experience bipolar disorder, and the average age of onset is 25, according to National Alliance on Mental Illness.
Advertisement
Professional Therapy, Done Online
A licensed therapist with BetterHelp can provide professional support and guidance, on your schedule. Sign up and get matched in as little as 48 hours.
Get Started
What Causes Depression?
Research suggests that a combination of biological, environmental, genetic and psychological factors play a role in causing depression. For example, factors such as a crisis, family history or substance abuse may trigger a major depressive episode. According to a 2022 World Health Organization study, the COVID-19 pandemic increased global rates of anxiety and depression by 25 percent.
Some people may simply develop depression with no apparent trigger.
- Stress
- Trauma
- Genetics
- Life circumstances – relationship changes, financial standing, etc.
- Medical conditions – chronic pain, sleep disturbances
- Attention-deficit/hyperactivity disorder – people with ADHD may also have depression
- Gender – women are more prone to depression than men
- Family history of depression
- Grief and loss
- Substance abuse
- Brain changes
- Poor diet
- Anxiety – people with anxiety may also suffer depression
How Does Clinical Depression Affect Different People?
Subsets of the population deal with depression differently and may have unique risks. Each group may require different types of therapy to help them cope.
Young Adults
Depression among young adults is on the rise. About 3.2 million young people ages 12 to 17 had at least one major depressive episode in 2017, according to the National Institutes of Mental Health.
Symptoms of depression in young people may differ from those in adults. For example, young people may experience moodiness, isolate themselves from adult family members and sleep at odd times of day. But they may still want to be with peers.
Symptoms also vary by gender. Girls are more likely to suffer from guilt, sadness, worthlessness and low energy. Boys are more likely to suffer from suicidal thoughts and irritability.
One study by Jean M. Twenge and colleagues analyzed data from 2005 to 2017 and found that rates of major depressive episodes had increased by 52 percent during that time among adolescents ages 12 to 17.
The authors theorized that cultural trends such as the “the rise of electronic communication and digital media and declines in sleep duration, may have had a larger impact on younger people.”
- National Suicide Hotline
- 1-800-273-8255
suicidepreventionlifeline.org - Crisis Textline
- Text “HELLO” to 741741
crisistextline.org
Men and Women
Men and women deal with depression differently, and more women than men suffer from depression. In fact, women are twice as likely to suffer from depression as men, according to the CDC.
Symptoms also manifest differently in women and men because of differences in hormone and gene development in the womb. Women tend to be better able to describe when they are depressed, so depression may not be diagnosed in men until later.
- Because of interactions between female hormones, women experience prolonged stress in response to difficult life events
- Men are more likely to commit suicide
- Substance abuse is more common in men with depression
- The illness is missed more frequently in men
- Women are more likely to have negative self-talk, to cry for no reason or blame themselves
About 2 to 5 percent of women may also suffer from premenstrual dysphoric disorder, or PMDD. PMDD is a severe form of premenstrual syndrome that can cause symptoms of depression. Some women require medication to treat it.
LGBTQ+ Individuals
Between 30 and 60 percent of LGBTQ+ individuals may suffer from depression and anxiety in their lives, according to Anxiety and Depression Association of America. Members of this community are up to 2.5 times more likely to suffer from mental illness than straight and gender-conforming individuals.
For example, according to the CDC’s Youth Risk Behavior Survey 2007 to 2017, 63 percent of lesbian, gay, bisexual and queer youth reported persistent feelings of sadness or hopelessness. About 47 percent seriously considered attempting suicide.
- The Trevor Project for LGBTQ+ youth in crisis
- Trained counselors are available 24/7 on the TrevorLifeline at 1-866-488-7386. The website also offers a chat and a text-for-help service. Text START to 678678 to start getting help.
- LGBTQ+ people can speak to trained volunteers about HIV/AIDS, coming out, safer sex, depression, suicide, harassment and violence. They can help connect callers with LGBT groups and services in your local area. LGBT Helpline (25+) 888-340-4528. Monday to Saturday, 6pm - 11pm / Peer Listening Line (25 & Under) 800-399-PEER. Monday to Saturday 5pm – 10pm.
Military and Veterans
Active-duty military and veterans have a higher risk of mental health disorders than civilians do.
In a study by Robert J. Ursano and colleagues, researchers found that the rate of major depression among soldiers was five times higher than the rate among civilians.
- 1 in 3 veterans has some symptoms
- 1 in 5 veterans has serious symptoms
- 1 in 8 to 10 has major depression requiring treatment
Veterans and military personnel dealing with depression can get help from their local VA hospital or visit the VA’s website.
Veterans in crisis can call the Veterans Crisis Line at 1-800-273-8255 and press 1, text to 838255, or chat online at VeteransCrisisLine.net/Chat.
Advertisement
Real Therapy, Done Online
BetterHelp offers flexible scheduling so you can make time for therapy in between meetings, classes, child care, and more. Get 20% off your first month.
Get Started
How to Deal with Depression
Most health care providers use a combination of therapies to treat depression. These include talk therapy, medications and lifestyle changes. The good news is that depression is highly treatable, and almost all patients find relief.
Because there is no one-size-fits-all treatment, some patients must go through a trial and error process with different medications and dosages or try different therapists. But according to the American Psychiatric Association, 80 to 90 percent of people eventually respond well to treatment.
Talk Therapy or Psychotherapy
There are several different types of psychotherapy. These include cognitive behavior therapy and intrapersonal therapy.
In research and clinical practice, cognitive behavior therapy, or CBT, has proven effective in treating depression and is endorsed by the American Psychiatric Association and American Psychological Association. The theory behind this type of therapy is that depression is based in part on unhelpful behaviors or thinking. A CBT therapist helps a patient learn better ways of coping with these behaviors and thoughts.
Interpersonal therapy, or IPT, has also been shown to be effective in major depressive disorders and is also endorsed by the American Psychiatric Association and American Psychological Association. IBT focuses on interpersonal issues and helps a patient learn to communicate better with others to address things that contribute to depression.
- Find a therapist that specializes in depression
- Check the therapist’s background and credentials
- Ask your therapist what their plan of treatment is and what happens if you don’t get better
- Find a few therapists you like and have a preliminary conversation with them to make sure you are comfortable with them
You can read more about different types of therapists and find one on the National Alliance on Mental Illness website.
Medications for Depression
There are several different types of medications to treat depression. Each drug class works differently and may have different risks and benefits. Medications can take between 2 to 4 weeks, or longer, to work.
It’s important not to stop taking a drug suddenly because you may suffer withdrawal side effects. If you want to stop taking your medication, work with your health care provider to slowly decrease the dose.
Make sure to ask your health care provider about side effects and tell them all medications, vitamins and herbal supplements you are taking.
| Drug Class | Name (generic) |
|---|---|
| Selective Serotonin Reuptake Inhibitors (SSRI) | Celexa (citalopram), Lexapro (escitalopram), Paxil (paroxetine), Prozac (fluoxetine), Trintellix (vortioxetine), Viibryd (vilazodone), Zoloft (sertraline) |
| Serotonin and Norepinephrine Reuptake Inhibitors (SNRI) | Cymbalta (duloxetine), Effexor (venlafaxine), Fetzima (levomilnacipran), Pristiq (desvenlafaxine) |
| Tricyclic and Tetracyclic Antidepressants | Ascendin (amoxapine), Elavil (amitriptyline), Ludiomil (maprotiline) |
| Atypical Antidepressants | Desyrel (trazodone), Serzone (nefazodone), Wellbutrin (bupropion) |
| Monoamine Oxidase Inhibitors (MAOIs) | Emsam skin patch (selegiline), Parnate (tranylcypromine), Marplan (isocarboxzaid) |
Natural Ways to Cope with Depression
Several lifestyle changes and activities can help individuals, their spouses and friends cope with depression. These involve connecting with others and taking care of your body.
- Care for a pet
- Caring for a pet can make you feel less isolated and take you out of your head.
- Join a support group
- Talking to others who can share their experience can help you feel less alone.
- Keep up with social activities
- Even if you don’t feel like being social, it’s important to connect with others. Being around others can help you feel less depressed.
- Support others
- Studies show volunteering and helping others gives us a sense of well-being and happiness.
- Look for a good listener
- It’s important to find someone who will listen without judgement and not try to “fix you.”
- Manage stress
- Identify things in life that stress you out and figure out how to take control of them or try deep breathing, meditation and yoga.
- Get enough sleep
- Any more or less than eight hours of sleep can trigger depression.
- Get exercise
- A study by Megan K. Edwards and Paul Loprinzi showed that a 10-minute bout of brisk walking and mediation improved mood.
- Get better nutrition
- Minimize sugar, eat more fruits and veggies and boost folate and omega-3 fatty acids. The American Psychiatric Association recommends folate and omega-3 fatty acids as adjunctive therapies for mood disorders.
Filing for Disability Benefits
Major depressive disorder is the number one cause of disability in United States. Some people who suffer from certain symptoms and limitations caused by depression can file for social security disability benefits.
In order to qualify, a person must have had depression for at least a year and be able to show that the symptoms prevent them from performing a job on a regular basis. The Social Security Administration will look at doctors’ notes, mental health evaluations, psychological testing and any other medical records.
- Slow physical movements and reactions
- Lack of interest in activities
- Depressed mood
- Thinking or concentration difficulties
- Feelings of guilt and worthlessness
- Difficulty sleeping or oversleeping
- Changes in weight caused by overeating or undereating
- Suicidal thoughts or thoughts of death
Find out more about social security disability on the Social Security Administration website.
Advertisement
Professional Therapy, Done Online
A licensed therapist with BetterHelp can provide professional support and guidance, on your schedule. Sign up and get matched in as little as 48 hours.
Get Started
Calling this number connects you with a Drugwatch.com representative. We will direct you to one of our trusted legal partners for a free case review.
Drugwatch.com's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.




